i.
Carrier tests:
In carrier tests, the carrier such as a silk or catgut thread or a penicylinder (a little stick) is contaminated
by submersion in a liquid culture of the test organism.
The carrier is then dried and is brought in contact with the disinfectant for a given exposure time. After the exposure, it is cultured
in a nutrient broth; no growth
indicates activity of the disinfectant tested whereas growth
indicates a failing.
Example of a carrier test is the in use-dilution test of the American Association of
Official Analytical Chemists (AOAC, 1990).
E.g. In Use-dilution test:
The AOAC Use-dilution test is a carrier-based test. The organisms
used are Salmonella cholerasuis, S. aureus and P. aeruginosa. Carriers (stainless
steel cylinders) are meticulously cleaned, sterilized by autoclaving in a
solution of aspargine, cooled and
inoculated with a test organism by immersing in
one of the culture suspensions. The cylinders are drained on filter paper, dried at 37°C for 40 minutes, exposed
to the use-dilution of the disinfectant for 10
minutes, and cultured
to assess the survival of the bacteria
ii. Suspension tests:
In these tests, a sample of the bacterial culture is suspended into the disinfectant solution and after exposure it is verified by
subculture whether this inoculum is killed
or not. Suspension tests are preferred
to carrier tests as the bacteria are uniformly exposed
to the disinfectant. There are different kinds of suspension tests:
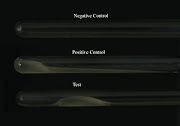
a. The qualitative suspension tests,
b. The quantitative suspension tests and
c. The test for the determination of the
phenol coefficient (Rideal and Walker, 1903)
a.
Qualitative test:
In this test, a loopful of bacterial suspension
is brought into contact with the disinfectant and again a loopful
of this mixture was cultured for
surviving organisms. Results are expressed as ‘growth’ or ‘no
growth’.
b.
Quantitative
methods:
In this
method, the number of surviving organisms is
counted and compared to the
original inoculum size. By
subtracting the logarithm of the
former from the logarithm of the latter, the decimal log reduction or microbicidal effect (ME) is obtained. An ME of 1 equals to a killing of 90% of the initial number of bacteria,
an ME of 2 means 99% killed.
A generally accepted
requirement is an ME that
equals or is greater than 5: at least 99.999% of the germs are killed.
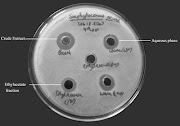
c. Phenol
coefficient test:
Phenol
coefficient may be defined as the
killing power of germicide or an antimicrobial agent towards a test organism compared
to that of phenol under identical conditions. It is the ratio
of the higher dilution of disinfectant killing the test organism in 10min. but not in 5min, to the of the highest
dilution of phenol showing the same result.
Procedure
— To a
series of dilutions of disinfectant being tested (5 ml per tube), 0.5 ml of
24hrs broth culture of test organism
(Staphylococcus aureus or Salmonella typhi) is added
— All tubes (disinfectant + organisms & phenol+ organisms)
are placed in 20°C water bath.
— At intervals of 5, 10 and 15 min, subcultures are made with a loop into sterile media tubes and
incubated for 48-72 hrs at 37°C and then observed for growth.
— The greatest dilution of disinfectant killing the test organism in 10 min
but not in 5 min is divided
by the greatest dilution of phenol showing the same result.
— The number obtained by this division is the phenol coefficient of the substance tested.
Table 1: Phenol coefficient method
|
Antimicrobial
agents
|
Dilutions
|
5 min
|
10
min
|
15
min
|
|
Disinfectant (X)
|
1:100
1:125
1:150
1:175
1:200
|
0
+
+
+
+
|
0
+ 0
+
+
|
0
0
0
0
+
|
|
Phenol
|
1:90
1:100
|
+
+
|
0
+
|
0
+
|
E.g. I: Rideal and Walker method;
It is developed by Rideal and Walker in 1903. In this technique, phenol is diluted from 1:400 to 1:800 and the
test disinfectant is diluted
from 1:95 to 1:115 and their bactericidal activity is determined against Salmonella typhi suspension.
Subcultures are performed from both
the test and phenol at intervals of 2.5,
5, 7.5 and 10 minutes. The plates are incubated
for 48-72 hours at 37°C.
That dilution of disinfectant
which disinfects the suspension in a given time is divided by that dilution
of phenol which disinfects the suspension in same
time gives its phenol coefficient.
Table 2: Rideal and Walker method
|
Disinfectant
|
Dilution
|
2.5
min
|
5 min
|
7.5min
|
10
min
|
|
Test disinfectant
|
1:400
1:500
1:600
1:700
1:800
|
NG G G G G
|
NG NG G G G
|
NG NG NG G G
|
NG NG NG NG G
|
|
Phenol
|
1:95
1:100
1:105
1:110
1:115
|
G G G G G
|
NG G G G G
|
NG NG G G G
|
NG NG NG NG G
|
Here, after 7.5
minutes, the test organism was killed by the test disinfectant at a dilution of 1:600. In the same period
the test organism was killed by phenol at a dilution of 1:100.
Phenol coefficient = 600/100 = 6
This result
indicates that the test disinfectant can be diluted six times as much as phenol and still
possess equivalent killing power for the test
organism
E.g. II: Chick Martin test
This test also determines the phenol coefficient of the test disinfectant. Unlike in Rideal-Walker method where the test is carried out in water, the disinfectants are made to act in the presence of yeast suspension (or 3% dried human feces) to simulate the presence of organic matter. Time for subculture is fixed at 30 minutes and the organism used to test efficacy is S. typhi as well as
S. aureus.
iii. In
capacity tests:
This test also determines the phenol coefficient of
the test disinfectant. Unlike in Rideal-Walker method where the test is carried out in water, the disinfectants are made to act in the presence of yeast suspension (or 3% dried human feces) to simulate the presence of organic matter. Time for subculture is fixed at 30 minutes
and the organism used to test efficacy is S. typhi as well as S. aureus.
In this method,
a soiled instrument is placed into a container with disinfectant; a certain quantity
of dirt and bacteria is added tothe
solution. The ability to retain
activity in the presence of an
increasing load is the capacity of the disinfectant. In a capacity test, the
disinfectant is challenged
repeatedly by successive additions of bacterial suspension until its capacity to kill has been exhausted. Capacity tests
simulate the practical situations of
housekeeping and instrument disinfection. The Best known capacity test is the
Kelsey-Sykes test (Kelsey and
Sykes, 1969).
E.g.
Kelsey and Sykes:
— It is
a triple challenge test, designed to determine
concentrations of disinfectant that
will be effective in clean and dirty condition
— The disinfectant is challenged by three successive additions of a bacterial suspension during the course of
the tests
— The concentration of the disinfectant is reduced by half by the addition of organic matter (autoclaved yeast cells), which builds
up to a final concentration of 0.5%
— Test organism used includes selected S. aureus, P. aeruginosa, P. vulgaris and E. coli
— The
method can be carried out under 'clean' or 'dirty‘conditions. The dilutions of the disinfectant are made in hard water for clean conditions and in yeast suspension for dirty conditions.
— Test organism
alone or with yeast is added at 0, 10 and 20 minutes interval. The contact time of disinfectant and test organism is 8 min.
— The
three sets of five replicate cultures
corresponding to each challenge are incubated at 320C for 48 hours and growth is assessed by turbidity.
— The
disinfectant is evaluated on its
ability to kill microorganisms or lack of it and the result is reported as a pass or a fail and not as a coefficient.
— Sets that contain two or more negative
cultures are recorded as a negative result.
— The disinfectant passes at the dilution
tested if negative results are
obtained after the first and second challenges.
— The third challenge
is not included in the pass/fail
criterion but positive
cultures serve as inbuilt
controls
Table 3: Kelsey and
Sykes method
|
Inoculum count
|
8 minute incubation
(1st set)
|
18 minute incubation (2nd set)
|
28 minute incubation (3rd set)
|
Result
|
|
2X109
|
+++++
|
+ + + + +
|
+
+ + + +
|
Fail
|
|
2X109
|
- - - - +
|
- - + + +
|
+ + + + +
|
Pass
|
|
2X109
|
- - - - -
|
- - - - -
|
- - - - +
|
Pass
|