MYCOLOGY
Fungi
are eukaryotic microorganisms with absorptive mode of nutrition, which do not
contain chlorophyll and reproduce by both asexual and sexual methods. The study
of fungi is called Mycology and the scientist who study fungi are called mycologists.
About 90,000 fungal species have already been described; however, some
estimates of total number suggest that 1.5 million species may exist.
TERMINOLOGY
USED IN MYCOLOGY
Some of the terminology used in
mycology is as follows.
A. Fungal element: Fungi
include unicellular yeast,
multicellular filamentous fungi called molds,
macroscopic puffballs, and mushrooms. The body or vegetative
structure of a fungus is called thallus. It varies in complexity and size,
ranging from the single cell microscopic yeast to multicellular molds,
macroscopic puffballs, and mushrooms. Fungi are eukaryotic microorganisms. The
fungal cell consists of cell wall made up of chitin, cytoplasmic membrane, and
other cell organelles (e.g. nucleus, ribosome, mitochondria etc.
B. Yeast: Yeast is a unicellular fungus that has a
single nucleus and reproduces either asexually by budding and transverse binary
fission or sexually through formation of spores (Ascospores). Each bud that
separates can grow into new yeast. Generally yeast cells are larger than
bacteria, vary considerably in size and are commonly spherical or egg
shaped. They do not have flagella but do
possess most of the other eukaryotic organelles. E.g. Saccharomyces spp., Candida
spp., Cryptococcus spp.
C. Molds:
Molds are multicellular filamentous fungi. E.g. Aspergillus, Mucor, Rhizopus
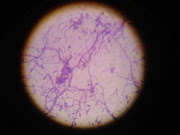
D. Hyphae:
Hyphae is the unit structure of filamentous fungi. Hyphae are composed of an
outer cell wall and inner lumen which contain the cytosol and cell organelles.
The hyphae of some fungi have cross walls called septa and called septate hyphae. Hyphae of other fungi
do not have septa and are called aseptate
or coenocytic hyphae.
E. Mycelium: Mycelium is the tangled mass of the
fungal hyphae of filamentous fungi.
F. Pseudomycelium or pseudohyphae or
sprout mycelium: A mycelium like structure consisting of
chains of cells formed by sequential budding is called pseudomycelium.
G. Germ tube: A
short, hyphae like structure which develops from certain types of spore on
germination or in yeast (e.g. Candida albicans) undergoing yeast to
mycelium transition. A germ tube usually develops into hyphae.
H. Rhizoids: Rhizopus (bread
molds) is fungi that grow in bread, vegetable, fruits, and other food products
and cause food spoilage. These molds produce clusters of root like holdfasts
which are called rhizoids. Morphologically, Rhizopus
has nonseptate, cottony mycelia with sporangiophores arising at the nodes where
the rhizoids form.
I. Dimorphic fungi: Many
fungi, especially those that cause diseases in humans and animals, are
dimorphic, i.e. they have two forms. Dimorphic fungi can change from the yeast
(Y) form in the animal to the mold or mycelial form (M) in the external
environment. E.g. Histoplasma capsulatum,
Blastomyces dermatidis etc.
J. Mycoses: Diseases
caused by fungi are called mycoses.
K. Dermatophytes: Three genera of
cutaneous fungi, Epidermophyton, Microsporum, and Trichophyton
which are are involved in cutaneous mycoses (skin, nail and hair infections)
are called dermatophytes.
Dermatophytic infections—also called dermatomycoses, ringworms, or tineas—occur worldwide and represent
the most common fungal diseases in humans.
·
Epidermophyton: Smooth
thin-walled Macroconidia only present, no microconidia, colonies a green-brown
to khaki color.
·
Microsporum: Macroconidia
with rough walls present, microconidia may also be present.
·
Trichophyton:
Microconidia present, smooth-walled macroconidia may or may
not be present.
GENERAL PROPERTIES OF
FUNGI
- They are
eukaryotic; cells contain membrane bound cell organelles including nuclei,
mitochondria, golgi apparatus, endoplasmic reticulum, lysosomes etc. They
also exhibit mitosis.
- Have
ergosterols in their membranes and possesses 80S ribosomes.
- Have a
rigid cell wall and are therefore non-motile, a feature that separates
them from animals. All fungi possess cell wall made of chitin.
- Are
chemoheterotrophs (require organic compounds for both carbon and energy
sources) and fungi lack chlorophyll and are therefore not autotrophic.
- Fungi are
osmotrophic; they obtain their nutrients by absorption.
- They obtain
nutrients as saprophytes (live off of decaying matter) or as parasites
(live off of living matter).
- All fungi
require water and oxygen and there are no obligate anaerobes.
- Typically
reproduce asexually and/or sexually by producing spores.
- They grow
either reproductively by budding or non-reproductively by hyphal tip
elongation.
- Food
storage is generally in the form of lipids and glycogen.
·
Table: Difference between bacteria and
fungi
FUNGI
|
BACTERIA
|
|
Cell type
|
Eukaryotic
|
Prokaryotic
|
Cell membrane
|
Sterol
present
|
Sterol
absent except in mycobacteria
|
Cell wall
|
Consists of chitin, mannans, glucans
|
Consists of peptidoglycan
|
Flagella, pili
|
Absent
|
Present
or absent
|
Reproduction
|
Sexual and asexual
|
Asexual
|
Spore formation
|
As
part of reproduction
|
For
survival in adverse condition
|
Metabolism
|
Heterotrophic
|
Autotrophic, heterotrophic
|
Oxygen requirement
|
Aerobic,
facultative anaerobic
|
Aerobic,
facultative anaerobic, microaerophilic, anaerobic
|
MORPHOLOGY OF FUNGI
Fungi exist in two
fundamental forms; the filamentous (hyphal) and single celled budding forms
(yeast). But, for the classification purpose they are studied as moulds,
yeasts, yeast like and dimorphic fungi.
Fungi exist in three
fundamental forms;
- Filamentous
and multicellular fungi (molds): The unit structure of filamentous
fungi is known as hyphae. Hyphae are composed of an outer cell wall and
inner lumen which contain the cytosol and cell organelles. The hyphae of
some fungi have cross walls called septa called septate hyphae. Hyphae of other fungi do not have septa and
are called aseptate or coenocytic
hyphae. The tangled mass of the fungal hyphae of filamentous fungi is
called Mycelium.
- Unicellular
fungi (yeast):
Yeast is a unicellular fungus that has a single nucleus and reproduces
either asexually by budding and transverse binary fission or sexually
through formation of Ascospores. Each bud that separates can grow into new
yeast. Generally yeast cells are larger than bacteria, vary considerably
in size and are commonly spherical or egg shaped. A typical yeast cell possesses most of
the other eukaryotic organelles. Some produce pseudohyphae and germ tube
(e.g. Candida spp.) and some are
capsulated (e.g. Cryptococcus
spp.). Yeast are separated on the basis of their size, shape, nature of budding,
and capacity to form pseudohyphae, capsule and germ tube.
- Dimorphic fungi (which occur both
as mold and yeast): Many fungi, especially those that cause
diseases in humans and animals, are dimorphic, i.e. they have two forms.
Dimorphic fungi can change from the yeast (Y) form in the animal to the
mold or mycelial form (M) in the external environment.
All fungi have typical
eukaryotic morphology. They have rigid cell wall composed of chitin, which may
be layered with mannans, glucans and other polysaccharides in association with
polypeptides. Some lower fungi possess cellulose in their cell wall. Some fungi
such as Cryptococcus and yeast form
of Histoplasma capsulatum possess polysaccharide capsules that help them
to evade phagocytosis.
Inner to the cell wall
is the plasma membrane that is a typical bi-layered membrane in addition to the
presence of sterols. Fungal membranes possess ergosterol in contrast to
cholesterol found in mammalian cells. The cytoplasm consists of various
organelles such as mitochondria, golgi apparatus, ribosomes, endoplasmic
reticulum, lysosomes, microtubules and a membrane enclosed nucleus. A unique
property of nuclear membrane is that it persists throughout the metaphase of
mitosis unlike in plant and animal cells where it dissolves and re-forms. The
nucleus possesses paired chromosomes.
Reproduction
in fungi and fungal spores:
Reproduction in fungi
can be either asexual or sexual.
Asexual reproduction is
accomplished in several ways.
- Asexual reproduction in
yeast takes place by
a. Fission
(a parent cell can divide into two daughter cells by central constriction and
formation of a new cell wall) or
b. Budding
(somatic vegetative cells may bud to produce new organisms.
- The most common method of
asexual reproduction in filamentous fungi is spore production. Asexual
spore formation occurs in an individual fungus through mitosis and
subsequent cell division. There are several types of asexual spores:
a. Arthroconidia
or
arthrospores: A hypha can
fragment (by the separation of hyphae through splitting of the cell wall or
septum) to form cells that behave as spores. These cells are called arthroconidia or arthrospores.
b. Chlamydospores:
If the cells are surrounded by a thick wall before separation, they are called chlamydospores.
c. Sporangiospores:
If the spores develop within a sac at a hyphal tip, they are called sporangiospores.
d. Conidiospores:
If the spores are not enclosed in a sac but produced at the tips or sides of
the hypha, they are termed conidiospores.
e. Blastospores Spores produced from a vegetative
mother cell by budding are called blastospores.
Sexual
reproduction in fungi involves the union of compatible nuclei. Some fungal
species are self-fertilizing and produce sexually compatible gametes on the
same mycelium (homothallic). Other species require out crossing between
different but sexually compatible mycelia (heterothallic). Depending on the
species, sexual fusion may occur between haploid gametes, gamete-producing
bodies called gametangia, or hyphae. This sexual reproduction yields
spores. E.g.:
a. Ascospores:
These single celled spores are produced in a sac called ascus. There are
usually eight ascospores in each ascus.
b. Basidiospores:
These single cell spores are produced on a club shaped structure called
basidium.
c. Zygospores:
Zygospores are large, thick walled spores formed when the tips of two sexually
compatible hyphae of certain fungi fuse together.
d. Oospores:
These are formed within a special female structure called oogonium.
Fertilization of the eggs by male gamete formed in an anthridium give rise to
oospores.
Fungal
spores are important for several reasons. The size, shape, color, and number of
spores are useful in the identification of fungal species. The spores are often
small and light; they can remain suspended in air for long periods. Thus they
frequently aid in fungal dissemination, a significant factor that explains the
wide distribution of many fungi.
DISTRIBUTION
OF FUNGI
Fungi are primarily terrestrial
organisms, although a few are freshwater or marine. Many are pathogenic and
infect plants and animals. Fungi also form association with other organisms.
The association of fungi with root of the higher plant is called mycorrhizae
and association between fungi and algae is called lichen.
IMPORTANCE
OF FUNGI
Fungi are important to humans in
both beneficial and harmful ways. They degrade complex organic materials in the
environment to simple organic compounds and inorganic molecules. In this way
carbon, nitrogen, phosphorus, and other critical constituents of dead organisms
are released and made available for living organisms. Besides this, fungi are
the major cause of plant disease. Over 5,000 species of fungi attack economically
valuable corps and garden plants and also many wild plants. Similarly many
diseases of animals and humans are caused by fungi. Some of the fungi have wide
industrial importance. Fungi play important role in making of bread, wine,
beer, cheese, soy sauce, and commercial production of many organic acids, ,
certain drugs (e.g. cortisone, cyclosporine) and many antibiotics (e.g.
penicillin). In addition, fungi are important research tools in the study of
fundamental biological processes. Cytologists, geneticists, biochemists,
biophysicists and microbiologists use fungi in research.
Beneficial
Effects of Fungi:
·
Decomposition
- nutrient and carbon recycling.
·
Biosynthetic
factories. The fermentation property is used for the industrial production of
alcohols, fats, citric, oxalic and gluconic acids.
·
Important
sources of antibiotics, such as Penicillin.
·
Model
organisms for biochemical and genetic studies. E.g.: Neurospora crassa
·
Saccharomyces cerviciae is extensively
used in recombinant DNA technology, which includes the Hepatitis B Vaccine.
·
Some
fungi are edible (mushrooms).
·
Yeasts
provide nutritional supplements such as vitamins and cofactors.
·
Penicillium
is used to flavour Roquefort and Camembert cheeses.
·
Ergot
produced by Claviceps purpurea contains medically important alkaloids that help
in inducing uterine contractions, controlling bleeding and treating migraine.
·
Fungi
(Leptolegnia caudate and Aphanomyces laevis) are used to trap
mosquito larvae in paddy fields and thus help in malaria control.
Harmful
Effects of Fungi:
·
Destruction
of food, lumber, paper, and cloth.
·
Animal
and human diseases, including allergies.
·
Toxins
produced by poisonous mushrooms and within food (Mycetism and Mycotoxicosis).
·
Plant
diseases.
·
Spoilage
of agriculture produces such as vegetables and cereals in the godown.
·
Damage
the products like magnetic tapes and disks, glass lenses, marble statues, bones
and wax.
Medically important fungi:
Among
90,000 species of fungi that have been described, fewer than 500 have been
associated with human disease, and about 100 are capable of causing infection
in normal individuals. The remainder of fungi produces disease in imunocompromized
hosts. Medical mycology is the discipline that deals with the fungi that
causes human disease. It should be noted that the importance of opportunistic
fungal pathogens is increasing because of the expansion of the imunocompromized
patient population.
Pathogenesis of fungal
diseases (Mycoses):
Most fungi are
saprophytic or parasitic to plants and are adapted to their natural
environment. Infection in humans is a chance event, occurring only when
conditions are favorable. Except for few fungi such as the dimorphic fungi that
cause systemic mycoses and dermatophytes, which are primary pathogens, the rest
are only opportunistic pathogens. Human body is a hostile environment and
offers great resistance to fungal invasion. Most fungi are saprophytic and
their enzymatic pathways function more efficiently at the redox potential of
non-living substrates than at the relatively more reduced state of living
metabolizing tissue. Some fungi such as Candida and Malasezzia have adapted to
human environment and exist as commensals.
The complex interplay
between fungal virulence factors and host defence factors will determine if a
fungal infection will cause a disease. Infection depends on inoculum size and
the general immunity of the host.
Virulence factors of
medically important fungi:
- Ability to
adhere to host cells by way of cell wall glycoproteins
- Production
capsules allowing them to resist phagocytosis
- Production
of a cytokine (e.g. GM-CSF) by Candida albicans that suppress the
production of complement.
- Ability to
acquire iron from red blood cells as in Candida albicans
- Ability to
damage host by secreting enzymes such as keratinase, elastase, collagenase
- Ability to
resist killing by phagocytes as in dimorphic fungi
- Ability to
secrete mycotoxins
- Having a unique
enzymatic capacity
- Exhibiting
thermal dimorphism
- Ability to
block the cell-mediated immune defences of the host.
Host defence factors:
- Physical
barriers, such as skin and mucus membranes
- The fatty
acid content of the skin
- The pH of
the skin, mucosal surfaces and body fluids
- Epithelial
cell turnover
- Normal
flora
- Chemical
barriers, such as secretions, serum factors
- Most fungi
are mesophilic and cannot grow at 37oC.
- Natural
Effector Cells (polymorphonuclear leucocytes) and the Professional
Phagocytes (monocytes and macrophages)
Factors predisposing to
fungal infections:
- Prolonged
antibiotic therapy
- Underlying
disease (HIV infection, cancer, diabetes, etc.)
- Age
- Surgical
procedures
- Immunosuppressive
drugs
- Irradiation
therapy
- Indwelling
catheters
- Obesity
- Drug
addiction
- Transplants
- Occupation
CLASSIFICATION
OF FUNGAL INFECTIONS (MYCOSES)
Taxonomic classification of fungi is complex and has little value in
clinical mycology laboratory. Among the large number of fungi identified, only
few may cause disease in human. In medical setting, medically important fungi
are categorized on the basis of basic morphology (e.g. yeast, mycelial fungi
and dimorphic fungi) and disease they cause (e.g. superficial mycoses,
cutaneous mycoses, subcutaneous mycoses and opportunistic mycosis.
Fungal infections are classified on the basis of the
site of infections. These fungal diseases, known as mycoses, are divided into five groups
according to the type of infected tissue in the host: superficial, cutaneous,
subcutaneous, systemic, and opportunistic mycoses.
1)
Superficial Mycoses
The
fungi responsible are limited to the outer surface of hair and skin and hence
are called superficial. The superficial mycoses mostly occur in the tropics.
Infections of the hair shaft are collectively called piedras (Spanish
for stone because they are associated with the hard nodules formed by mycelia
on the hair shaft). For example, black piedra is caused by Piedraia
hortae and forms hard black nodules on the hairs of the scalp. White
piedra is caused by the yeast Trichosporon beigelii and forms
light-colored nodules on the beard and mustache. Some superficial mycoses are
called tineas [Latin for grub, larva, worm], the specific type being
designated by a modifying term. Tineas are superficial fungal infections
involving the outer layers of the skin, nails, and hair. Tinea versicolor is
caused by the yeast Malassezia furfur and forms brownish-red scales on
the skin of the trunk, neck, face, and arms. Treatment involves removal of the
skin scales with a cleansing agent and removal of the infected hairs. Good
personal hygiene prevents these infections.
2)
Cutaneous Mycoses
Cutaneous
mycoses—also called dermatomycoses, ringworms, or tineas—occur worldwide
and represent the most common fungal diseases in humans. Three genera of
cutaneous fungi, or dermatophytes, are involved in these mycoses: Epidermophyton,
Microsporum, and Trichophyton. Diagnosis is by microscopic
examination of biopsied areas of the skin cleared with 10% potassium hydroxide
and by culture on Sabouraud dextrose agar. Treatment is with topical ointments
such as miconazole, tolnaftate, or clotrimaz for 2 to 4 weeks. Griseofulvin and
itraconazole are the only oral fungal agents currently approved by the FDA for
treating dermatophytoses.
·
Tinea barbae [Latin barba, the beard] is an
infection of the beard hair caused by Trichophyton mentagrophytes or T.
verrucosum. It is predominantly a disease of men who live in rural areas
and acquire the fungus from infected animals.
·
Tinea capitis [Latin capita, the head]
is an infection of the scalp hair. It is characterized by loss of hair,
inflammation, and scaling. Tinea capitis is primarily a childhood disease
caused by Trichophyton or Microsporum species. Person to-person
transmission of the fungus occurs frequently when poor hygiene and overcrowded
conditions exist. The fungus also occurs in domestic animals, from whom it can
be transmitted to humans. A Wood’s light (a UV light) can help with the
diagnosis of tinea capitis because fungus-infected hair fluoresces when
illuminated by UV radiation.
·
Tinea corporis [Latin corpus, the body]
is a dermatophytic infection of the smooth or bare parts of the skin. The
disease is characterized by circular, red, well-demarcated, scaly,
vesiculopustular lesions accompanied by itching. Tinea corporis is caused by Trichophyton
rubrum, T. mentagrophytes, or Microsporum canis. Transmission of the
disease is by direct contact with infected animals or humans or by indirect
contact through fomites.
·
Tinea cruris [Latin crura, the leg] is a
dermatophytic infection of the groin. The pathogenesis and clinical
manifestations are similar to those of tinea corporis. The responsible fungi
are Epidermophyton floccosum, T. mentagrophytes, or T. rubrum. Factors
predisposing one to recurrent disease are moisture, occlusion, and skin trauma.
·
Tinea pedis [Latin pes, the foot], also known
as athlete’s foot, and tinea manuum [Latin mannus, the
hand] are dermatophytic infections of the feet and hands, respectively.
Clinical symptoms vary from a fine scale to a vesiculopustular eruption.
Itching is frequently present. Warmth, humidity, trauma, and occlusion increase
susceptibility to infection. Most infections are caused by T. rubrum, T.
mentagrophytes, or E. floccosum. Tineapedis and tinea manuum occur
throughout the world, are most commonly found in adults, and increase in
frequency with age.
·
Tinea unguium [Latin unguis, nail] is a
dermatophytic infection of the nail bed. In this disease the nail becomes
discolored and then thickens. The nail plate rises and separates from the nail
bed. Trichophyton rubrum or T. mentagrophytes are the causative
fungi.
3)
Subcutaneous Mycoses
The
dermatophytes that cause subcutaneous mycoses are normal saprophytic
inhabitants of soil and decaying vegetation. Because they are unable to
penetrate the skin, they must be introduced into the subcutaneous tissue by a
puncture wound that has been contaminated with soil containing the fungi. Most
infections involve barefooted agricultural workers. Once in the subcutaneous
tissue, the disease develops slowly—often over a period of years. During this
time the fungi produce a nodule that eventually ulcerates and the organisms
spread along lymphatic channels producing more subcutaneous nodules. At times
such nodules drain to the skin surface. The administration of oral
5-fluorocytosine, iodides, amphotericin B, and surgical excision are the usual
treatments. Diagnosis is accomplished by culture of the infected tissue.
- One type of
subcutaneous mycosis is chromoblastomycosis. The nodules are
pigmented a dark brown. This disease is caused by the black molds Phialophora
verrucosa or Fonsecaea pedrosoi. These fungi exist worldwide,
especially in tropical and subtropical regions. Most infections involve
the legs and feet.
- Another
subcutaneous mycosis is maduromycosis, caused by Madurella
mycetomatis, which is distributed worldwide and is especially
prevalent in the tropics. Because the fungus destroys subcutaneous tissue
and produces serious deformities, the resulting infection is often called
a eumycotic mycetoma or fungal tumor. One form of mycetoma, known
as Madura foot, occurs through skin abrasions acquired while walking
barefoot on contaminated soil.
- Sporotrichosis
is
the subcutaneous mycosis caused by the dimorphic fungus Sporothrix
schenckii. The disease occurs throughout the world and is the most
common subcutaneous mycotic disease in the United States. The fungus can
be found in the soil, on living plants, such as barberry shrubs and roses,
or in plant debris. Infection occurs by a puncture wound from a thorn or
splinter contaminated with the fungus. The disease is an occupational
hazard to florists, gardeners, and forestry workers. After an incubation
period of 1 to 12 weeks, a small red papule arises and begins to ulcerate.
New lesions appear along lymph channels and can remain localized or spread
throughout the body, producing extracutaneous sporotrichosis.
4)
Systemic Mycoses
Except
for Cryptococcus neoformans, which has only a yeast form, the fungi that
cause the systemic or deep mycoses are dimorphic—that is, they exhibit a
parasitic yeastlike phase (Y) and a saprophyticmold or mycelial phase (M). Most
systemic mycoses are acquired by the inhalation of spores from soil in which
the mold-phase of the fungus resides. If a susceptible person inhales enough
spores, an infection begins as a lung lesion, becomes chronic, and spreads
through the bloodstream to other organs (the target organ varies with the
species).
- Blastomycosis
is
the systemic mycosis caused by Blastomyces dermatitidis, a fungus
that grows as budding yeast in humans but as a mold on culture media and
in the environment. The disease occurs in three clinical forms: cutaneous,
pulmonary, and disseminated. The initial infection begins when
blastospores are inhaled into the lungs. The fungus can then spread
rapidly, especially to the skin, where cutaneous ulcers and abscess
formation occur. B. dermatitidis can be isolated from pus and
biopsy sections. Diagnosis requires the demonstration of thick-walled,
yeast like cells 8 to 15 μm in diameter. Complement-fixation,
immunodiffusion, and skin (blastomycin) tests are also useful.
Amphotericin B, itraconazole, or ketoconazole are the drugs of choice for
treatment. Surgery may be necessary for the drainage of large abscesses.
- Coccidioidomycosis,
also
known as valley fever, San Joaquin fever, or desert rheumatism, is caused
by Coccidioides immitis. C. immitis exists in the dry, highly
alkaline soils of North, Central, and South America. In the soil and on
culture media, this fungus grows as a mold that forms arthroconidia at the
tips of hyphae. In humans the fungus grows as a yeast-forming, thick-walled
spherule filled with endospores. Most cases of coccidioidomycosis are
asymptomatic or indistinguishable from ordinary upper respiratory
infections. Almost all cases resolve themselves in a few weeks, and a
lasting immunity results. A few infections result in a progressive chronic
pulmonary disease. The fungus also can spread throughout the body,
involving almost any organ or site. Diagnosis is accomplished by
aspiration and identification of the large spherules (approximately 80 μm
in diameter) in pus, sputum, and aspirates. Culturing clinical samples in
the presence of penicillin and streptomycin on Sabouraud agar also is
diagnostic. Newer methods of rapid confirmation include the testing of
supernatants of liquid media cultures for antigens, serology, and skin
testing. Miconazole, itraconazole, ketoconazole, and amphotericin B are
the drugs of choice for treatment. Prevention involves reducing exposure
to dust (soil) in endemic areas.
- Cryptococcosis
is
a systemic mycosis caused by Cryptococcus neoformans. This fungus
always grows as large budding yeast. In the environment C. neoformans is
a saprophyte with a worldwide distribution. Aged, dried pigeon droppings
are an apparent source of infection. Cryptococcosis is found in
approximately 15% of AIDS patients. The fungus enters the body by the
respiratory tract, causing a minor pulmonary infection that is usually
transitory. Some pulmonary infections spread to the skin, bones, viscera,
and central nervous system. Once the nervous system is involved, cryptococcal
meningitis usually results. Diagnosis is accomplished by detection of the
thick-walled spherical yeast cells in pus, sputum, or exudate smears using
India ink to define the organism. The fungus can be easily cultured on
Sabouraud dextrose agar. Identification of the fungus in body fluids is
made by immunologic procedures. Treatment includes amphotericin B or
itraconazole. There are no preventive or control measures.
- Histoplasmosis
is
caused by Histoplasma capsulatum var. capsulatum, a
facultative parasitic fungus that grows intracellularly. It appears as small
budding yeast in humans and on culture media at 37°C. At 25°C it grows as
a mold, producing small microconidia (1 to 5 μm in diameter) that are
borne singly at the tips of short conidiophores. Large macroconidia or
chlamydospores (8 to 16 _m in diameter) are also formed on conidiophores.
In humans the yeast like form grows within phagocytic cells. H.
capsulatum var. capsulatum is found as the mycelial form in
soils throughout the world and is localized in areas that have been
contaminated with bird or bat excrement. The chlamydospores, particularly
the microconidia, are easily spread by air currents. Histoplasmosis is an
occupational disease among spelunkers (people who explore caves) and bat
guano miners. Humans acquire histoplasmosis from airborne microconidia
that are produced under favorable environmental conditions. Histoplasmosis
is a disease of the monocyte-macrophage system; thus many organs of the
body can be infected. More than 95% of cases have either no symptoms or
mild symptoms such as coughing, fever, and joint pain. Lesions may appear
in the lungs and show calcification; most infections resolve on their own.
Only rarely does the disease disseminate. Laboratory diagnosis is
accomplished by complement fixation tests and isolation of the fungus from
tissue specimens. Currently the most effective treatment is with
amphotericin B, ketoconazole, or itraconazole. Prevention and control
involve wearing protective clothing and masks before entering or working
in infested habitats. Soil decontamination with 3 to 5% formalin is
effective where economically and physically feasible.
E)
Opportunistic Mycoses
An
opportunistic microorganism is generally harmless in its normal
environment but becomes pathogenic in a compromised host. A compromised host
is seriously debilitated and has a lowered resistance to infection. There
are many causes of this condition, among them the following: malnutrition;
alcoholism; cancer, diabetes, leukemia, or another infectious disease; trauma
from surgery or injury; an altered microbiota from the prolonged use of
antibiotics (e.g., in vaginal candidiasis); and immunosuppression by drugs,
viruses (HIV), hormones, genetic deficiencies, chemotherapy of patients, and
old age. The most important opportunistic mycoses include systemic aspergillosis,
candidiasis, and Pneumocystis carinii pneumonia.
- Aspergillosis: Of all the
fungi that cause disease in compromised hosts, none are as widely
distributed as the Aspergillus species. Aspergillus is
omnipresent in nature, being found wherever organic debris occurs. Aspergillus
fumigatus is the usual cause of aspergillosis. A. flavus is
the second most important species, particularly in invasive disease of
immunosuppressed patients. The major portal of entry for Aspergillus is
the respiratory tract. Inhalation of conidiospores can lead to several
types of pulmonary aspergillosis. One type is allergic aspergillosis.
Infected individuals may develop an immediate allergic response and suffer
typical asthmatic attacks when exposed to fungal antigens on the
conidiospores. In bronchopulmonary aspergillosis the major clinical
manifestation of the allergic response is bronchitis. Although tissue
invasion seldom occurs in bronchopulmonary aspergillosis, Aspergillus often
can be cultured from the sputum. A most common manifestation of pulmonary
involvement is the occurrence of colonizing aspergillosis, in which Aspergillus
forms colonies within the lungs that develop into “fungus balls”
called aspergillomas. These consist of a tangled mass of mycelia growing in
a circumscribed area. From the pulmonary focus, the fungus may spread,
producing disseminated aspergillosis in a variety of tissues and organs.
In patients whose resistance has been severely compromised, invasive
aspergillosis may occur and fill the lung with fungal mycelia. Laboratory
diagnosis of aspergillosis depends on identification, either by direct
examination of pathological specimens or by isolation and characterization
of the fungus. Successful therapy depends on treatment of the underlying
disease so that host resistance increases. Treatment is with itraconazole.
- Candidiasis
is
the mycosis caused by Candida albicans and other species Candida. In contrast to the other
pathogenic fungi, C. albicans is a member of the normal microbiota
within the gastrointestinal tract, respiratory tract, vaginal area, and
mouth (see figure 31.2). In healthy individuals C. albicans does
not produce disease. However, if anything upsets the normal microbiota, Candida
may multiply rapidly and produce candidiasis. Recently Candida species
have become important nosocomial pathogens. In some hospitals they may
represent almost 10% of nosocomial bloodstream infections. No other
mycotic pathogen produces as diverse a spectrum of disease in humans as
does C. albicans. Most infections involve the skin or mucous
membranes (Oral candidiasis; onychomycosis; Intertriginous;
candidiasis; Napkin (diaper) candidiasis; Candidal vaginitis; balanitis).
This occurs because C. albicans is a strict aerobe and finds such
surfaces very suitable for growth. Cutaneous involvement usually occurs
when the skin becomes overtly moist or damaged. Besides this, Candida can
cause many systemic infections. Diagnosis of candidiasis is difficult
because (1) this fungus is a frequent secondary invader in diseased hosts,
(2) a mixed microbiota is most often found in the diseased tissue, and (3)
no completely specific immunologic procedures for the identification of Candida
currently exist. There is no satisfactory treatment for candidiasis.
Cutaneous lesions can be treated with topical agents such as sodium
caprylate, sodium propionate, gentian violet, nystatin, miconazole, and
trichomycin. Ketoconazole, amphotericin B, fluconazole, itraconazole, and
flucytosine also can be used for systemic candidiasis.
- Pneumocystis
carinii pneumonia:
Pneumocystis
carinii are
eucaryotic protists found in the lungs of a wide variety of mammals. The
natural history of P. carinii is poorly understood, in large part
because of a lack of a continuous in vitro culture system for its
propagation. Although it was once considered a protozoan parasite, recent
comparisons of rRNA and DNA sequences from several genes have shown that P.
carinii is more closely related to fungi than protozoa. The disease
that this protist causes, pneumocystis pneumonia or Pneumocystis
carinii pneumonia (PCP), occurs almost exclusively in
immunocompromised hosts. Extensive use of immunosuppressive drugs and
irradiation for the treatment of cancers and following organ transplants
accounts for the formidable prevalence rates noted recently. This
pneumonia also occurs in more than 80% of AIDS patients. Both the organism
and the disease remain localized in the lungs—even in fatal cases. Within
the lungs Pneumocystis causes the alveoli to fill with a frothy
exudate. Laboratory diagnosis of pneumocystis pneumonia can be made
definitively only by microscopically demonstrating the presence of the
microorganisms in infected lung material or by a PCR analysis. Treatment
is by means of oxygen therapy and either combination of trimethoprim and
sulfamethoxazole, atovaquone, or trimetrexate. Prevention and control is
through prophylaxis with drugs in susceptible persons.
LABORATORY
DIAGNOSIS OF FUNGAL INFECTION
- Introduction
- Selection
of specimens
- Collection
of specimens (Skins,
nails and hairs; Mucous membrane; Ear; Eye; Blood; CSF; Urine;
Exudates/pus; Stool; Other body fluids (peritoneal, pericardial,
synovial); Lower respiratory tract specimens; Bone marrow; Tissue)
- Specimen
transport and storage
- Specimen
processing
- Laboratory
analysis and interpretation (Direct microscopic examination;
Culture; Histopathological examination; Mycoserology; Molecular diagnosis)
1.
Introduction
General
approach: Diagnosis is based on the
combination of clinical observation and laboratory investigation. Diagnosis
solely based on clinical basis has limited value;
·
It
is not unusual to find that the appearance of lesion has been modified and
rendered atypical by previous treatment in case of superficial infection
·
The
clinical presentation of deep infection is non specific and can be caused by a
wide range of infections, underlying illness or complication of treatment
·
Radiological
or other imaging methods are relied upon to distinguish fungal infection from
other cause of infection.
Role
of laboratory analysis
·
Confirming
the clinical diagnosis of fungal infection
·
Antifungal
susceptibility testing
·
Providing
objective assessment of response to treatment
·
Monitoring
resolution of the treatment
The
successful diagnosis of fungal infection depends on the collection of
appropriate specimens and selection of appropriate microbiological test
procedures. The laboratory findings can sometimes be unhelpful or even
misleading
·
Close
liaison between the clinician and the laboratory is particularly important.
·
The
clear demarcation between classical pathogen and saprophytic fungi no longer
exist in imunocompromized patients.
2. Selection of specimens
·
Selection
of specimen differs from mycoses to mycoses as well as the presenting symptoms
and clinical signs.
·
The
specimen must contain viable etiological agent if it is to be recovered and
identified.
·
Must
be collected in such a manner that it will allow the fungus to remain viable in
its natural state, with no contamination.
3. Collection of specimens
Inappropriately
collected/ transported or processed specimen leads to
·
Misdiagnosis/
under diagnosis
·
Delay
in appropriate therapy
·
Increased
cost of the patients
General
guidelines for specimen collection
·
Appropriate
site
·
The
specimen should be collected from active lesions, old lesions often do not
contain viable organisms
·
Appropriate
volume
·
Appropriate
time
·
Collect
the specimen under aseptic condition
·
Collect
sufficient specimens
·
Collect
specimen before initiating therapy
·
Use
sterile collection devices/ container (not required for skin, nail and hairs)
·
Label
the specimen appropriately
·
Collect
sufficient background information from patients
Collection
procedures for some specimens are as follows
3.1 Skins, nails and hairs
- Should be collected in folded
square of black paper (10 x10cm)
- Prior cleaning of superficial
lesions with 70% alcohol prior to sampling (especially if ointments,
creams, or powder have been applied to lesions).
- Fungal agents: Dermatophytes, Candida spp, Trichosporon spp.
Collection of
skin:
·
Should
be collected from cutaneous lesions by scraping outward from the margin of the
lesion with scalpel.
·
Use
of adhesive disc (if there is scaling of lesion)
Collection of
hairs:
·
Use
of wood’s light/ or collect lusterous hairs or stumps/ or hairs broken off al
follicle mouth
·
Pluck
hais with forceps (cut hairs without root is unsuitable).
·
Brushing
of scalp with plastic massage pad (for patient’s with incospicious scalp
lesions)
Nail specimens:
·
Should
be taken from any discoloured, distrophic or brittle part of nails
·
Specimen
should be cut far back as possible from the edge and should be of full
thickness of nail.
·
Scrapping
can be taken if nail is thickened.
3.2 Mucous
membrane
- Scrappings from oral lesions are
better than swabs.
- In case of veginal infections, swab
should be taken from discharge in the vegina and from the lateral veginal
wall.
- Swabs should be moistened with
saline or sterile water prior to collection and sent in transport media.
- Fungal agents: Candida spp, C. immitis
3.3 Ear
- Scrappings of material from the ear
canal are to be preferred than swab.
- Fungal agents: filamentous fungi
3.4 Eye
- For corneal ulcer: scrap the ulcer
with sterile platinum spatula/ swabs are not suitable.
- Endoopthalmitis: collect vitreous
humour
- Fungal agents: filamentous fungi, C. albicans, C. neofarmans
3.5 Blood
- Preferred in all cases of suspected
deep fungal infections.
- Specialized technique or media are
used for isolation of fungi other than Cryptococcus
neoformans, Trichosporon
spp. and Candida spp.
- Isolation of fungi from blood
depends on number of factors:
ü Amount of blood
ü Number of sample
collected
ü Method of processing
·
Collection
of arterial blood is considered if venous blood culture is unsuccessful.
·
Isolation
rates are high when the medium is vented and aerated, use of biphasic media,
use of lysis centrifugation system, automated blood culture system.
- Fungal agents: H capsulatum, C. neoformans, Candida spp.
3.6. Cerebrospinal fluid
- Ideal volume: 3-5 ml
- Centrifugation and use of sediment
for culture/ microscopy is effective, supernatant can be used for serology
and biochemistry.
- Fungal agents: C. neoformans
3.6 Urine
- Fresh MSU specimes (50- 100 ml) are
used for non catheterized patients
- Suprapubic aspiration for children
- Collect urine specimen after
prostatic massage for blastomycosis and cryptococcosis.
- Urine specimens are processed for
direct microscopy, culture and fungal antigen.
- Fungal agents: yeast, C. immitis, H. capsulatum, B.
dermatidis
3.7 Stool
- Requred for profound
immunosupressed bone marrow transplant recipients.
- Collect rectal swab or stool in
sterile container.
3.8 Pus/ exudates
- Swabs are not suitable to collect
material draining abscess or ulcer (if used should be taken from as deep
as possible).
- Pus from draining abscess or sinus
should be aspirated
- Grains if visible should be
collected.
- Fungal agents: yeast and
filamentous fungi, actinomycetes
3.9 Other body
fluids
·
Peritoneal,
pericardial, synovial fluids can be collected from drainage or by aspiration
with heparin (heparin is not used for patients with continuous peritoneal
dialysis).
·
Fungal
agents: H capsulatum, C. neoformans
3.10 Lower respiratory tract specimens
·
Early
morning sputum samples, at least three samples
·
Should
be processed within two hours of collection (if delay store at 4˚C)
·
Induced
sputum (using nubelized serum)
·
Bronchoalveolar
lavage (BAL) or bronchial washing
·
Percutaneous
needle biopsies for patients with focal lung disease.
·
Fungal
agents: yeast and filamentous fungi, actinomycetes
3.11 Bone marrow
- Used for histoplasmosis,
cryptococcosis, paracoccidiomycosis
- About 3-5 ml, collect in container
with heparin.
- Fungal agents: H capsulatum, C. neoformans
3.12 Tissue
- Collect specimen form both edge and
middle of the lesions
- Should be placed in sterile saline
and not in formalin.
- Fungal agents: yeast and
filamentous fungi, actinomycetes
3.13 Specimens for serological tests/ drug level
determination
- Paired or sequential samples are
more appropriate
- Blood, CSF, urine or other fluid
are used
- Collect without anticoagulants
4. Specimen
transport and storage
·
All
clinical specimens should be analyzed promptly as far as practicable (except
for suspected dermatophytosis).
·
If
processing is going to be delayed, incubate normally sterile specimens (e.g.
blood, CSF) at 37˚C and specimens that are potentially contaminated with
bacterial contamination (e.g.. Aspirates, pus, urine, sputum) at 4˚C but do not
froze.
·
H. capsulatum doesn’t survive
for long periods under refrigeration. Limited studies have shown significantly
decreased viability of H. capsulatum, C
immitis, B. dermatidis and A.
fumigatus stored at room temperature or on dry ice.
·
Transport
media are not needed except for blood and corneal scrapings.
·
Specimens
should not be frozen before culture.
·
Transported
specimen should never be allowed to dry.
·
Specimen
mailed to laboratories should follow transport guidelines.
5.
Specimen processing
- Concentration by centrifugation
- Highly viscous specimen such as
sputum should be liquified before culture
- Homogenization in tissue grinder
6.
Laboratory analysis and interpretation
- The choice of the appropriate tests
differs from one disease to another and depends on the site of infection
as well as the presenting symptoms and clinical signs. The investigation
used for fungal diagnosis includes:
6.1
Direct microscopic examination
- Simpler and must helpful procedure
for fungal diagnosis.
- Most useful in diagnosis of
cutaneous and subcutaneous mycosis; can stabilize the diagnosis of deep
mycoses.
- Helps to determine whether an
organism recovered later in culture is a contaminant or pathogenic and to
assist the laboratory in selecting the most appropriate culture conditions
to recover organism visualized on direct smear.
- Unstained wet mount preparation can
be examined by bright field, dark field or pahase contrast microscopy.
- Various methods can be used:
ü Calcofluor white for detecting fungi, requires
fluorescence microscope.
ü Giemsa stain for examining bone marrow and
peritoneal blood smears to detect intracellular H. capsulatum
ü Grams stains
for detecting yeast cells/ bacteria
ü India ink for detecting Cryptococcus neoformans in CSF and other body fluids
ü Methylene blue for detecting fungi in skin
scrapping
ü Potassium hydroxide for clearing
specimen to make fungi more visible
ü Methanamine silver stain for detecting
fungi in histological specimens
ü Papanicolaou stain for examining secretion for
presence of malignant cell to detect fungal elements
ü PAS stain for detecting fungi
ü Wright stains for examining bone marrow and
peripheral blood smear for detection of intracellular H. capsulatum.
·
The
sensitivity of direct microscopy depends on the quality of specimens, specimen
type, quality of microscope, and quality of microscopist in recognizing fungal
elements and their diagnostic morphology. Characteristics of fungal elements in
clinical specimens are as follows.
Morphology
|
Organism
|
Size(µm)
|
Characteristics
|
Yeast
|
Blastomyces
dermatidis
Cryptococcus neoformans
Histoplasm
capsulatum var.
capsulate
Paracoccidioides
brasiliensis
Sporothrix
schenckii
|
8-18
2-15
2-5
5-60
2-6
|
Usually large and spherical double retractile,
buds usually single and connected by broad base, small forms (2-5µm) may be
seen.
Cells vary in size, usually spherical but may be
football shaped, buds usually single and pinched off, capsule may or may not
be evident, pseudohyphal forms with or without capsule are rarely seen.
Small, oval to round budding cells, often found
clustered within histocytes,, difficult to detect when present in small
number
Cells usually large and surrounded by smaller buds
around periphery (mariner’s wheel appearance), smaller cell that resembles Histoplasma may be present, buds have
pinched off appearance.
Small, oval to round to cigar shaped, single or multiple
buds present, often not seen in clinical specimens.
|
Yeast form or pseudohyphae or true hyphae
|
Candida
spp.
|
3-4
(5-10)
|
Cells usually exhibit single budding, pseudohyphae
when present are constricted at ends and remain attached like links of sausage,
true hyphae when present have parallel walls and are septate
|
Yeast forms and hyphae
|
Malassezia
furfur
|
3-8
(2.5-4)
|
Short, curved hyphal elements, usually present
along with round yeast cells that retain their spherical shapes in compacted
clusters when found in skin
|
Spherules
|
Coccidioides
immitis
|
10-200
|
Vary in size, some contains endospores, other are
empty. Adjacent spherules may resemble B.
dermatidis and endospore may resemble H.
capsulatum. Hyphae may be found.
|
Hyaline, septate hyphae
|
Dermato-phytes
Aspergillus
spp.
Fusarium spp.
|
3-15
3-12
3-12
|
Presence of chain of arthroconidia
Hyphae withdichotomous branching (45˚)
Septate hyphae, impossible to distinguish from
other hyaline molds
|
Phaeoid septate hyphae
|
Phialophora
spp.
|
2-6
|
Budding cells with single septa and chains of
swollen rounded cells may be present. Occasionally aggregates may be present.
|
Muriform bodies
|
Phialophora
verrucosa
|
5-20
|
Round to pleomorphic thick walled cells with
transverse septa, Cells commonly contain two fission plates that form a
tetrad of cell, occasionally bhanched septate hyphae
|
Granules
|
Fusarium
spp.; and Aspergillus nidulans
|
200-500
|
White soft granules with cement like matrix
|
Sprongia
|
Rhinisporidium
seeberi
|
6-300
|
Large thick walled sporangia containing sporangiophore
|
Wide, non septate hyphae
|
Zygomycetes
|
10-30
|
Hyphae are large, ribbon like, often fractured or
twisted. Occasionally septa may present, branching usually at right angle.
Smaller hyphae overlap with those of Aspergillus,
particularly A. flavus.
|
6.2
Culture
- Isolation in culture permit must
pathogenic fungi to be identified
- The laboratory must be aware of the
particular fungal agents that are suspected in a given sample so that the
most appropriate media can be included
6.2.1.
Culture media:
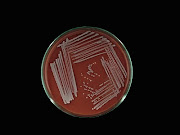
Specimens are generally inoculated onto primary isolation
media, like Sabouraud's dextrose agar and Brain heart infusion agar
supplemented with 5% sheep blood. Several media are available.
·
Cornmeal Glucose Sucrose Yeast Extract Agar for
Zygomycetes To stimulate sporulation in some zygomycetes, especially Saksenaea and Apophysomyces.
·
Brain Heart Infusion Agar (BHIA) with 5% Sheep Blood For the primary isolation and cultivation of yeasts
and moulds.
·
Trichophyton
Agars Nos 2-7For the differentiation of Trichophyton species.
·
Littman
Oxgall Agar For routine inoculation of specimens from skin, nails,
hair etc.
·
Sabouraud's
Dextrose Agar with 5% NACL For the cultivation and
differentiation of dermatophytes especially T. rubrum from T. mentagrophytes.
·
CGB
(L-Canavanine, glycine, 2 bromthymol blue) Agar For distinction between Cryptococcus neoformans var. neoformans and Cryptococcus neoformans var. gattii.
6.2.2 Inoculation, Culture condition
6.2.2.1
Cerebrospinal Fluid (CSF):
·
The specimen should be centrifuged. Keep the
supernatant for cryptococcal antigen testing and process the sediment as
follows.
·
For
direct microscopy use 1 drops of the sediment to make an India ink mount.
·
Resuspend the remaining sediment in 1-2 ml of
CSF and inoculate onto; (a) SDA with chloramphenicol and gentamicin and incubate
duplicate cultures at 26˚C and 35˚C; and (b) Brain heart infusion agar (BHIA)
supplemented with 5% sheep blood and incubate at 35˚C. Maintain cultures for at
least 4 weeks.
6.2.2.2
Sputum, Bronchial Washings and Throat Swabs
·
Unless it is already sufficiently fluid, sputa
may need to be emulsified by shaking with about 3-5ml of sterile distilled
water, depending on the volume of the original specimen. Any bits of blood, pus
or necrotic material should be plated directly onto media.
·
Make wet mount preparations in KOH (l drop) and
Gram stained smears (l drop) of all suspicious areas. The PAS stain may be
necessary if the KOH preparation is unsatisfactory.
·
Inoculate sample onto: (a) Sabouraud's dextrose
agar with chloramphenicol and gentamicin and incubate duplicate cultures at
26˚C and 35˚C; and (b) Brain heart infusion agar (BHIA) supplemented with 5%
sheep blood and incubate at 35˚C. Maintain cultures for 4 weeks.
6.2.2.3 Skin Scrapings and Swabs
Skin scrapings, nail scrapings and epilated hairs where tinea
is the provisional diagnosis:
·
Make a wet mount preparation in KOH for direct
microscopy. Note a Calcofluor stained mount may also be necessary.
·
Inoculate specimen onto two slopes containing
cycloheximide i.e. one DERMASEL agar slope and one LACTRITMEL agar slope also
containing chloramphenicol, gentamicin and incubate cultures at 26˚C. Maintain
cultures for 4 weeks.
·
Where a moistened swab has also been collected
from the same site as the scraping, inoculate this onto a Sabouraud's dextrose
agar slope containing chloramphenicol and gentamicin, but NO cycloheximide and
incubate at 26˚C. Maintain cultures for 4 weeks.
Skin scrapings and swabs where
candidiasis is the provisional diagnosis:
A. Skin scrapings:
·
Make a wet mount preparation in KOH for direct
microscopy. Note a Calcofluor stained mount may also be necessary.
·
Inoculate specimens onto Sabouraud's dextrose
agar slopes containing chloramphenicol and gentamicin, but NO cycloheximide and
incubate at 35˚C. Maintain cultures for 4 weeks.
B. Skin swabs:
·
Smear swab onto heat sterilized glass slide for
Gram stain.
·
Inoculate specimens onto Sabouraud's dextrose
agar containing chloramphenicol and gentamicin, but NO cycloheximide and
incubate at 35˚C. Maintain cultures for 4 weeks.
·
Where secondary bacterial infection is
suspected, and separate swabs for routine bacteriology were not collected, the
swab should first be inoculated onto a blood agar plate, followed by the
Sabouraud's agar containing the antibiotics and then placed into Brain Heart
Infusion Broth. All cultures should be incubated at 35˚C. Maintain cultures for
4 weeks.
Scrapings from the groin, feet or
nails where either a dermatophyte or Candida
species may be isolated. This includes the possibility of a non-dermatophyte
onychomycosis.
·
Direct Microscopy:
Wet mount preparation in KOH for direct microscopy. Note a Calcofluor stained
mount may also be necessary.
·
Inoculate specimens onto Sabouraud's dextrose
agar containing chloramphenicol and gentamicin, but NO cycloheximide (as for Candida) and incubate at 26C. Maintain
cultures for 4 weeks.
·
Inoculate specimen onto a DERMASEL agar slope
containing cycloheximide, chloramphenicol and gentamicin and incubate cultures
at 26˚C. Maintain cultures for 4 weeks.
·
Where a moistened swab has also been collected
from the same site as the scraping, inoculate this onto a Sabouraud's dextrose
agar slope containing chloramphenicol and gentamicin, but NO cycloheximide and
incubate at 26C. Maintain cultures for 4 weeks.
Skin scrapings from patients with
suspected Pityriasis versicolor:
·
Direct
Microscopy: Wet mount preparation in KOH for direct microscopy along with
the cellotape stripping taken at the time of collection.
·
Inoculate scrapings onto a DIXON'S agar slope
for isolation of Malassezia furfur and incubate cultures at 26˚C.
Maintain cultures for 4 weeks.
·
Inoculate specimen onto Sabouraud's dextrose
agar with chloramphenicol and gentainicin but NO cycloheximide and incubate
cultures at 26˚C. Maintain cultures for 4 weeks.
·
If dermatophytes are to be excluded also inoculate
onto DERMASEL agar slope and incubate cultures at 26˚C. Maintain cultures for 4
weeks.
Skin scrapings from patients where
a systemic pathogen is suspected:
·
Direct
Microscopy: Wet mount preparation in KOH for direct microscopy. Note a
Calcofluor stained mount may also be necessary.
·
Inoculate specimens onto: (a) Sabouraud's
dextrose agar with chloramphenicol and gentamicin but NO cycloheximide and
incubate duplicate cultures at 26˚C and 35˚C; and (b) Brain heart infusion agar
(BHIA) supplemented with 5% sheep blood and incubate at 35˚C. Maintain cultures
for 4 weeks.
6.2.2.4
Blood and Bone Marrow
·
Special media are necessary for the optimum
recovery of fungi.
·
Numerous blood culture systems are available;
however all systems must be vented to atmospheric air and incubated at 30˚C to
maximize the rate and time of recovery of fungal organisms.
·
Prepare several smears for Giemsa, Gram and PAS
staining. Culture the remaining specimen by one or more of the following
methods. With bone marrow aspirates the initial material is generally used for
making smears for Giemsa staining, the remaining 3-5 ml of marrow and blood may
be cultured on the media listed below.
·
Cultures should be maintained for 4 weeks.
·
Direct culture method:
Inoculate 0.5-1.0 ml of buffy coat, prepared by centrifuging 5-10 ml of blood,
onto the surface of the media. This inoculum can then be spread over the
surface of the agar with a sterile inoculating loop and the plate incubated
aerobically at 30˚C.
·
Biphasic culture bottle: A
ratio of 1:10 to 1:20 (blood to broth) is recommended, a minimum of 5.0 ml of
blood is required for each culture bottle. The biphasic culture bottle is kept
vented and is tilted daily to allow broth to flow over the agar surface. These
cultures must be carefully checked daily for growth. Because fungi will not
turn the broth very cloudy it is imperative to frequently Gram stain the bottle
contents to detect fungal elements.
·
Membrane filter technique:
Briefly, specimens are treated sequentially with Triton-X and sodium carbonate
solutions to lyse blood cells and then filtered by vacuum through a 0.45 um
membrane. This membrane is then placed onto the media.
·
Lysis centrifugation isolator system:
The Isolator utilizes a tube that contains components that lyse leukocytes and
erythrocytes and also inactivate plasma complement and certain antibiotics.
Once lysed, the cells release the microorganisms contained within them, and the
centrifugation step in the procedure serves to concentrate the organisms in the
blood sample. This concentrate is then inoculated onto the surface of
appropriate culture media.
·
Bactec: Bactec have produced a
special fungal media (BACTEC Fungal Medium) for enhanced fungal blood culture
using their non-radiometric (NR) instruments. Once again, blood cells are lysed
by the medium to enhance recovery of fungi. Note antimicrobials have also been
added to limit the growth of bacteria.
·
Primary isolation media for blood and
bone marrow culture: (a) Sabouraud's dextrose agar with
chloramphenicol and gentamicin and incubate duplicate cultures at 26˚C and
35˚C; and (b) Brain heart infusion agar (BHIA) supplemented with 5% sheep blood
and incubate at 35˚C. Maintain cultures for 4 weeks.
6.2.2.5 Tissue Biopsies from Visceral Organs
·
If areas of pus and necrosis are present,
inoculate directly onto the isolation media. Also perform a smear for direct
microscopic examination.
·
If there are no areas of pus or necrosis then
process the specimen by mincing it into pieces as small as possible with a
sterile scalpel blade, or for soft tissues by grinding in a sterile glass
tissue grinder and inoculate onto the media.
·
Warning: zygomycetous fungi
will not survive the chopping up or tissue grinding process.
·
For direct microscopy examination of tissue
sections stained with H&E, GMS & PAS is essential. Direct smears may
also be made by smearing a small amount of tissue onto slides for Gram stain.
·
Inoculate onto: (a) Sabouraud's dextrose agar
with chloramphenicol and gentamicin and incubate duplicate cultures at 26˚C and
35˚C; and (b) Brain heart infusion agar (BHIA) supplemented with 5% sheep blood
and incubate at 35˚C. Maintain cultures for 4 weeks.
·
Note: Negative bacteriological
cultures from patients with clinical evidence of an infection should be sealed
with tape and maintained at 26˚C for 4 weeks to exclude the presence of a slow
growing fungus.
6.2.2.6
Urine
·
Yeasts recovered from routine urine bacteriology
cultures of catheterized urine or urine obtained by sterile procedure should be
identified and reported regardless of colony count. However, the isolation of
yeasts from clean catch specimens must be interpreted with caution and is not
significant without additional support from other clinical and laboratory
investigations.
·
Note: Negative bacteriological
cultures from patients with clinical evidence of an infection should be sealed
with tape and maintained at 26˚C for 4 weeks to exclude the presence of a slow
growing fungus.
·
Centrifuge the urine for 10-15 minutes at 2000
rpm. Decant the supernatant and pool the sediment if necessary.
·
Prepare a direct smear of the sediment in KOH
for direct microscopy. Note PAS, Gram or India ink preparations may also be
helpful.
·
Inoculate 0.05-0.1 ml of the sediment onto
Sabouraud's agar with gentamicin and chloramphenicol and incubate duplicate
cultures at 26˚C & 35˚C. Maintain cultures for 4 weeks.
6.3
Identification of culture: Key Features include Microscopic
Morphology and Culture Characteristics:
Blastomyces dermatitidis
·
On Sabouraud's dextrose agar at 25˚C, colonies
are variable in both morphology and rate of growth. They may grow rapidly,
producing a fluffy white mycelium, or slowly as glabrous, tan, non-sporulating
colonies.
·
Microscopically, hyaline, ovoid to pyriform,
one-celled, smooth-walled conidia (2-10 um in diameter) are borne on short
lateral or terminal hyphal branches.
·
On blood agar at 37˚C, colonies are wrinkled and
folded, glabrous and yeast-like. Microscopically, the organism produces the
characteristic yeast phase as seen in tissue pathology. B. dermatitidis
can be described as a dimorphic fungus.
Coccidioides
immitis/posadasii
complex
·
The two species are morphologically identical
and can be distinguished only by genetic analysis and different rates of growth
in the presence of high salt concentrations (C. posadasii grows more
slowly).
·
C. immitis is geographically limited to
California’s San Joaquin Valley region, whereas C. posadasii is found
in the desert regions of the USA southwest, Mexico and South America. The two
species appear to coexist in the desert regions of the USA southwest and
Mexico.
·
Colonies of C. immitis/posadasii on
Sabouraud’s dextrose agar at 25˚C are initially moist and glabrous, but rapidly
become suede-like to downy, greyish white with a tan to brown reverse, however
considerable variation in growth rate and culture morphology has been noted.
·
Microscopy shows typical single-celled, hyaline,
rectangular to barrel-shaped, alternate arthroconidia, 2.5-4 x 3-6 µm in size,
separated from each other by a disjunctor cell.
Histoplasma capsulatum
·
H. capsulatum exhibits thermal
dimorphism by growing in living tissue or in culture at 37˚C as a budding
yeast-like fungus or in soil or culture at temperatures below 30˚C as a mould.
·
On Sabouraud's dextrose agar at 25˚C, colonies
are slow growing, white or buff-brown, suede-like to cottony with a pale
yellow-brown reverse. Other colony types are glabrous or verrucose, and a red
pigmented strain has been noted.
·
Microscopic morphology shows the presence of
characteristic large (8-14 um in diameter), rounded, single-celled, tuberculate
macroconidia formed on short, hyaline, undifferentiated conidiophores.
Microconidia, if present, are small (2-4 um in diameter), round to pyriform and
borne on short branches or directly on the sides of the hyphae.
·
On brain heart infusion (BHI) blood agar
incubated at 37˚C, colonies are smooth, moist, white and yeast-like.
Microscopically, numerous small round to oval budding yeast-like cells, 3-4 x
2-3 um in size are observed.
·
Three varieties of H. capsulatum are
recognized, depending on the clinical disease: var. capsulatum is the
common histoplasmosis, var. duboisii is the African type and var. farciminosum
causes lymphangitis in horses. Histoplasma isolates may also resemble species
of Sepedonium and Chrysosporium.
Paracoccidioides
brasiliensis
·
On Sabouraud's dextrose agar at 25˚C, colonies
are slow growing and variable in morphology. Colonies may be flat, wrinkled and
folded, glabrous, suede-like or downy in texture, white to brownish with a tan
or brown reverse.
·
Microscopically, a variety of conidia may be
seen, including pyriform microconidia, chlamydoconidia and arthroconidia.
However, none of these are characteristic of the species, and most strains may
grow for long periods of time without the production of conidia.
·
On BHI blood agar at 37˚C, the mycelium converts
to the yeast phase and colonies are white to tan, moist and glabrous and become
wrinkled, folded and heaped. Microscopically, numerous large, 20-60 um, round,
narrow base budding yeast cells are present. Single and multiple budding
occurs, the latter are thick-walled cells that form the classical
"steering wheel" or "Mickey mouse" structures that are
diagnostic for this fungus, especially in methenamine silver stained tissue
sections.
Hyaline
Hyphomycetes
·
Hyaline Hyphomycetes include those conidial
fungi which are not darkly pigmented; colonies may be colorless or brightly
colored. These include the agents of hyalohyphomycosis, Aspergillosis,
dermatophytosis and the dimorphic pathogens, like Histoplasma capsulatum.
·
Identification of the hyphomycetes is primarily
based on microscopic morphology including; (a) conidial morphology, especially
septation, shape, size, color and cell wall texture; (b) the arrangement of
conidia as they are borne on the conidiogenous cells (c) the type conidiogenous
cell
·
Culture characteristics, although less reliable
may also be useful. These include surface texture, topography and
pigmentation, reverse pigmentation and growth at 37˚C. For
identification, potato dextrose agar and cornmeal agar are two of the most
suitable media to use and exposure to daylight is recommended to maximize
culture color characteristics.
·
Mandatory to see conidial characteristics to
make an identification therefore must have a good slide preparation [needle
mounts, tape mounts, slide cultures]. May also need to stimulate
sporulation by using different media, such as potato dextrose agar or cornmeal
agar.
Aspergillus spp.
·
Aspergillus colonies are usually fast
growing, white, yellow, yellow-brown, brown to black or shades of green, and
they mostly consist of a dense felt of erect conidiophores.
·
Conidiophores terminate in a vesicle covered
with either a single palisade-like layer of phialides (uniseriate) or a layer
of subtending cells (metulae) which bear small whorls of phialides (the
so-called biseriate structure). The vesicle, phialides, metulae (if
present) and conidia form the conidial head. Conidia are one-celled, smooth-
or rough-walled, hyaline or pigmented and are basocatenate, forming long dry
chains which may be divergent (radiate) or aggregated in compact columns
(columnar).
·
For identification, isolates are usually
inoculated at three points on Czapek dox agar and potato dextrose agar and
incubated at 25˚C. Most species sporulate within 7 days.
·
Descriptions are primarily based on colony
pigmentation and morphology of the conidial head. Microscopic mounts are
best made using a cello tape flag or slide culture preparation mounted in
lactophenol cotton blue. A drop of alcohol is usually needed to detach
the cellotape flag from the stick, and to act as a wetting agent.
·
Key Features: Hyaline
hyphomycete showing distinctive conidial heads with flask-shaped phialides
arranged in whorls on a vesicle.
Fusarium spp.
·
Colonies are usually fast growing, pale or
brightly colored (depending on the species) and may or may not have a cottony
aerial mycelium. The color of the thallus varies from whitish to yellow,
brownish, pink, reddish or lilac shades.
·
Species of Fusarium typically produce both
macro- and microconidia from slender phialides. Macroconidia are hyaline, two-
to several-celled, fusiform to sickle-shaped, mostly with an elongated apical
cell and pedicellate basal cell. Microconidia are 1- to 2-celled, hyaline,
pyriform, fusiform to ovoid, straight or curved. Chlamydoconidia may be present
or absent.
·
Identification of Fusarium species is
often difficult due to the variability between isolates (e.g. in shape and size
of conidia and colony color) and because features that are required are not
always well developed (e.g. the absence of macroconidia in some isolates after
subculture). .
Dematiaceous
Hyphomycetes
ü
Dematiaceous Hyphomycetes are those conidial
fungi that produce dark brown, green-black, or black colonies and are the
causative agents of phaeohyphomycosis. These includes: Acrophialophora, Alternaria, Aureobasidium, Bipolaris, Cladophialophora, Cladosporium, Curvularia, Drechslera, Epicoccum, Exophiala, Exserohilum, Fonsecaea, Hortaea, Lecythophora, Ochroconis, Phaeoacremonium, Phialophora, Pithomyces, Ramichloridium, Rhinocladiella, Scedosporium, Sporothrix, Stemphylium, Ulocladium, Veronaea
Dermatophytes
·
Microscopic morphology of the micro and/or
macroconidia is the most reliable identification character, but needs good
slide preparation and to stimulate sporulation in some strains.
·
Culture characteristics such as surface texture,
topography and pigmentation are variable and are therefore the least reliable
criteria for identification.
·
Clinical information such as the site,
appearance of the lesion, geographic location, travel history, animal contacts
and race is important, especially in identifying rare non-sporulation species
like M. audouini, T. concentricum and T schoenleinii
etc.
·
Epidermophyton:
Smooth thin-walled Macroconidia only present, no microconidia, colonies a green-brown to khaki colour.
Smooth thin-walled Macroconidia only present, no microconidia, colonies a green-brown to khaki colour.
·
Microsporum:
Macroconidia with rough walls present, microconidia may also be present.
Macroconidia with rough walls present, microconidia may also be present.
·
Trichophyton:
Microconidia present, smooth-walled macroconidia may or may not be present.
Microconidia present, smooth-walled macroconidia may or may not be present.
Sporothrix schenckii
·
At 25˚C, colonies are slow growing, moist and
glabrous, with a wrinkled and folded surface. Some strains may produce short
aerial hyphae and pigmentation may vary from white to cream to black.
·
Conidiophores arise at right angles from the
thin septate hyphae and are usually solitary, erect and tapered towards the
apex. Conidia are formed in clusters on tiny denticles by sympodial
proliferation of the conidiophore, their arrangement often suggestive of a
flower.
·
As the culture ages, conidia are subsequently
formed singly along the sides of both conidiophores and undifferentiated
hyphae. Conidia are ovoid or elongated, 3-6 x 2-3 um in size, hyaline,
one-celled and smooth-walled.
·
In some isolates, solitary, darkly pigmented,
thick-walled, one-celled, obovate to angular conidia may also be observed along
the hyphae.
·
On BHI blood agar at 37˚C, colonies are
glabrous, white to greyish yellow and yeast-like, consisting of spherical or
oval budding yeast cells.
Yeasts
(Blastoschizomyces, Candida, Cryptococcus, Loboa loboa, Malassezia, Rhodotorula, Saccharomyces, Trichosporon)Identification.
·
Yeast-like fungi may be basidiomycetes, such as Cryptococcus
neoformans or ascomycetes such as Candida albicans.
ü
Germ Tube Test: lightly
inoculated 5 ml of serum, containing 0.5% glucose and incubated at 35˚C for 2-3
hours.
ü Positive = Candida
albicans or Candida dubliniensis.
- Negative or from HIV
positive patient = perform assimilation tests.
·
For the identification of germ tube negative
yeasts, morphological (Dalmau plate culture), physiological and biochemical
tests are essential.
Candida spp.
·
The genus Candida is characterized by
globose to elongate yeast-like cells or blastoconidia that reproduce by
multilateral budding.
·
Most Candida species are also
characterized by the presence of well developed pseudohyphae, however this
characteristic may be absent, especially in those species formally included in
the genus Torulopsis.
·
Within the genus Candida, fermentation,
nitrate assimilation and inositol assimilation may be present or absent,
however, all inositol positive strains produce pseudohyphae.
·
CHROMagar Candida plate showing chromogenic
colour change for C. albicans (green), C. tropicalis (blue), C.
parapsilosis (white) and C. glabrata (pink).
- Candida albicans,
Candida colliculosa,
Candida dubliniensis,
Candida fabianii, Candida famata, Candida glabrata,
Candida guilliermondii, Candida haemulonii, Candida
inconspicua, Candida keyfyr, Candida krusei,
Candida lipolytica, Candida lusitaniae,
Candida norvegensis,
Candida parapsilosis,
Candida pelliculos, Candida rugosa, Candida tropicalis, Candida viswanathii
Cryptococcus
·
The genus Cryptococcus is characterized
by globose to elongate yeast-like cells or blastoconidia that reproduce by
multilateral budding. Pseudohyphae are absent or rudimentary.
·
On solid media the cultures are generally mucoid
or slimy in appearance. Red, orange or yellow carotenoid pigments may be
produced, but young colonies of most species are usually non-pigmented, and are
cream in color.
·
Most strains have encapsulated cells with the extent of capsule formation depending
on the medium. Under certain conditions of growth the capsule may contain
starch-like compounds which are released into the medium by many strains.
·
Within the genus Cryptococcus,
fermentation of sugars is negative, assimilation of nitrate is variable and
assimilation of inositol is positive. The genus Cryptococcus is
similar to the genus Rhodotorula. The distinctive difference between
the two is the assimilation of inositol, which is positive in Cryptococcus.
6.3
Mycoserology
- Useful in early diagnosis of
systemic fungal infection.
- Agglutination, precipitation,
complement fixation and enzyme immunoassay are widely used.
- Detection
of antibodies
ü Includes most of
the currently available standardized procedures
ü Limited value in
diagnosing imunocompromized patients.
ü Useful in
diagnosing fungal disease, such as histoplasmosis and coccidioidomycosis.
- Detection
of antigens is now becoming more widely available. Stablished
for diagnosis of cryptococcosis and histoplasmosis and being evaluated for
other fungi.
- Antigen
detection methods are complicated
ü Often released
in minute amount necessitating the use of highly sensitive test procedure
ü Often cleared
very rapidly necessitating frequent collection of samples
ü Often bound to
circulating IgG
- The result of the serological
testing are seldom more than suggestive or supportive of a fungal
diagnosis and must be interpreted with clinical and laboratory finding.
Disease
|
Test
antigens
|
Interpration
|
Aspergillosis
|
CF (Aspergillin)
A. fumigatus, A. niger and A. flavus
ID, aspergillin
|
Titre ≥1:32 is suggestive of infection
Higher titer have a stronger correlation with
disease
Multiple precipitation bands increase the
suspicion of active disease. Positive in 95% of cases with fungus ball, 50%
with bronchopulmonarry disease. May be positive in invasive disease rarely.
|
Blastomycosis
|
Cf, yeast form
ID, yeast culture filtrate
EIA, extract of B. dermatidis
|
Titre of ≥1:8 are significant. Higher titer are
more indicative of disease. Cross reaction occur with histoplasmosis and
coccidioidomycosis. High percentages of cases are negative.
Specific band for A antigen. Many culture proven
cases are negative.
A positive relative value suggests disease.
Sensitive than ID
|
Candidiasis
|
ID, C
albicans sonicate
LA, yeast cytosol or mannan
|
Most cases have bands, however high percentage of
normal populations have antibody to C. albicans
≥1:4 or ≥1:8 are considered positive, difficult to
interpret, most have clinical correlation
|
Cryptococcosis
|
LA, Ab to capsular polysaccharide
EIA, Ab to capsular polysaccharide
|
Detects cryptococcal capsular polysaccharide. Any
titer significant. RF causes false positive.
More
sensitive than LA
|
Histoplasmosis
|
CF,histoplasmin (mycelia)
CF, yeast cell
ID histoplasmin
EIA, H. capsulatum
|
≥1:8 is significant. Higher titer paralles more
severity.
≥1:8 is significant. Higher titer paralles more
severe disease. May cross react with blastomyces and coccidioidomycosis
Specific band on H and M antigen. M bands usually
appear first in disease and persist. H band is associated with active disease
& often dissociates with active therapy.
A positive relative EIA value indicates disease.
Tests for IgG. More sensitive than ID.
|
Sporotrichosis
|
LA yeast
|
Titre ≥1:80 usually indicate active disease.
Usually negative with systemic sporotricosis.
|
6.3
Histopathological examination of tissue section
- Most reliable procedure for the
diagnosis of subcutaneous and deep seated fungal infection.
- In addition to culture and serology
histopathology is the important means of diagnosis of fungal infection.
- When the mycosis is not suspected,
whole specimen is often fixed for histopathology, in such cases
histopathology is the only means of fungal diagnosis.
- Recognition of fungal pathogen in
tissue specimen depends on its abundance and distinctiveness in
appearance.
- Stains
ü Hematoxylin and
eosin-may be insufficient to reveal fungal elements.
ü Methenamine
silver (Gomori/ Grocott) and Periodic acid Schiff are specific
·
Fungal
genus may not be identified in all cases only by staining.
·
Histopathological
studies can sometimes confirms the possibility of multiple infections or
exclude a fungal disease from clinical differential diagnosis.
·
Immunoperoxidase
and immunoflourescence staining are available for some fungi.
·
DNA
probe based methods are under investigation.
6.5
Molecular diagnosis
- Numerous methods: for the detection
of fungal nucleic acid in clinical specimens (esp. Blood, CSF, Respiratory
specimens etc).
- Polymerase chain reaction based
methods are common and widely used.
ü Conventional
PCR, Multiplex PCR, Nested PCR, Real
time PCR
- Several regions within the genome
have been evaluated as potential targets: mostly ribosomal DNA gene complex
(18S, 5.8 S and 28S).
SOME
PRACTICAL TECHNIQUE
Preparation of 20% KOH – glycerol solution:
Potassium hydroxide is
a strong alkali used as a clearing agent to observe fungi in the specimen in a
wet mount preparation for specimen such as sputum, pus, urine sediment,
homogenate from biopsy tissue, nail, hair, etc., to clear cell debris. The
formula consists of
- KOH – 20 g
- Glycerol –
20 ml
- Distilled
water – 80 ml
(1) The
relative amounts of KOH and distilled water must be adjusted according to the
percentage of KOH used.
(2) Addition
of glycerol to KOH solution will prevent crystallization occurring in the
solution, thus enhancing the shelf life of this reagent. It will also permit
keeping the KOH preparation for a couple of days before it drys.
Preparation of Sabouraud dextrose agar (SDA):
This modification
differs from the original formula in that it has an approximately neutral pH
and contains only 2% dextrose. The original medium (with high sugar, up to 40%
and low pH of 5.4) devised by Raymond Sabouraud is more suitable for isolation
and study of dermatophytes.
- Dextrose –
20 g
- Neopeptone
– 10 g
- Agar – 15 g
- Distilled
water-1000 ml.
Preparation:
The ingredients are mixed and dissolved by boiling and then autoclaved. After
autoclaving dispence in sterile petriplates of fungul cultute bottle (make
slant). This formulation is available in prepared or dehydrated form. The final
pH is around 6.8 (near neutral).
Storage:
The prepared medium can be stored at 4˚C.
KOH mounts preparation:
Potassium hydroxide is
a strong alkali used as a clearing agent to observe fungi in the specimen in a
wet mount preparation. 10%-20% KOH is usually used depending on the specimen;
occasionally 40% is also used when not cleared by 10%-20% KOH. Used for
specimen such as sputum, pus, urine sediment, homogenate from biopsy tissue,
nail, hair, etc., to clear cell debris.
Preparation of the
mount
(1)
Take a clean grease-free glass slide.
(2)
Place a large drop of KOH solution with
a Pasteur pipette.
(3)
Transfer small quantity of the specimen
with a loop or the tip of a scalpel into the KOH drop.
(4)
Put a clean cover slip over the drop
gently so that no air bubble is trapped.
(5)
Place the slide in a moist chamber, and
keep at room temperature.
(6)
Tissue usually takes 20-30 minutes;
sometimes overnight contact with KOH is useful for getting a positive result.
(7)
Clearing can be hastened by gentle
heating of the slide, but it is best avoided.
Observation
1.
Examine the clear specimen under low
power (10X or 20X objective). Scan the entire cover slip from end to end in a
zigzag fashion.
2. If
any fungal elements are suspected, examine under high power (40X objective).
3. Reduce
the light coming into the condenser while examining at high power.
4.
Look for budding yeast cells, branching
hyphae, type of branching, the colour, septation and thickness of hyphae.
Modification
For more distinction,
stains like methylene blue or Parker blue-black fountain ink may be used along
with KOH. This will impart a colored background and fungal elements, if
present, will show as prominent refractile objects.
Advantages
·
Simple, economical and rapid
Disadvantages
·
Pus
and sputum may contain artifacts, which may superficially resemble hyphal and
budding forms of fungi. These artifacts may be produced by cotton or wool
fibres, starch grains (in pleuritis) or cholesterol crystals.
·
It
gives an idea about the presence of hyphal element, but cannot distinguish
different fungi.
·
Preparation
cannot be kept for too long; but drying can be prevented/prolonged by keeping
the slides in a moist chamber (covered Petri dish with a wet filter paper on
which a triangular glass rod is placed).
Precautions
(1)
The drop of KOH should not be so large
that the cover slip floats.
(2)
If kept outside a moist chamber, the KOH
dries and crystals form that restrict the visibility of the fungus.
(3)
After clearing, pressure is to be gently
applied on the top of the cover slip with a fold of filter paper or the handle
of a teasing needle. This ensures even spreading of the material onto the
slide.
(4)
KOH should be kept in a closed container
in small aliquots ready to use on the workbench.
Quality
assurance
Fungal spores or hyphae
may contaminate the KOH solution kept in the laboratory and may give false
positive results. A negative control should therefore be put up every day.
India ink or nigrosin
preparation for C. neoformans
It is the simple methods to identify the
capsulated varieties of Cryptococcus neoformans.
Procedure:
(1)
The preparation should be made in the
centre of a clean, grease free glass slide.
(2)
Put 1 drop of India ink or Nigrosin on
the centre of the slide. Too much stain makes the background too dark. (Upon
examination, if the staining appears too dark, a small amount of water may be
applied on the edge of the cover slip and the cover slip gently tapped: this will
dilute the stain to some extent.)
(3)
Put 1 loopful of the specimen or
preferably centrifuge sediment from the fluid specimen to be tested (e.g. CSF,
spinal fluid, urine, and other body fluids) close to the drop of the stain.
(4)
Mix the two well with the loop, or
preferably a sterile needle. The loop should be cooled before use; otherwise
the stain tends to precipitate.
(5)
Hold the cover slip vertically such that
one edge just touches the fluid on the slide. The fluid will spread along the
edge by surface tension.
(6)
Keeping that edge in contact with the
fluid surface, drop the cover slip gently on the fluid, so that no air bubble
is trapped inside. If there are air bubbles, the surface of the cover slip may
be gently tapped by the needlepoint, so as to move the bubbles towards the
edge. But this should be avoided as far as possible.
(7)
Examine slide immediately under the
microscope. Since the stain tends to dry fast in air, if immediate examination
is not feasible, the slide should be kept in a moist chamber.
Observation:
Scan the entire cover
slip from end to end in a zigzag fashion. Encapsulated yeast cells (Cryptococcus
neoformans) are seen under low power as luminous dots in an otherwise dark
background. Under high power, the cells can also be seen, containing refractile
bodies, and surrounded by the unstained thickness of the capsule.
Characteristic pinched-off budding, when observed, is confirmatory for
diagnosis.
Please note
§ Besides the
classical budding-yeast form, various unusual forms can also be seen, including
elongated forms that look like pseudohyphae; this is mainly due to a very high
multiplication rate of the organism in HIV/AIDS patients.
§ In the very late
stage in progressive AIDS, it may be difficult to differentiate the capsules of
individual cells; the organism may remain enmeshed in a matting of the capsular
material.
§ Micro- or
non-capsulated strains of the organism are also reported on rare occasions. In
such cases, gram stain of the sample is helpful in identification.
§ The edges of the
cover slip should be specially examined. When placing the cover slip, the yeast
cells tend to move towards the periphery along with the fluid. For this reason
the common practice of draining the extra fluid from the sides should be
avoided.
§ If the protein
content of the CSF is too high, India ink sometimes may form floccules, which
make it difficult to demonstrate the capsule.
§ In the case of
Nigrosin stain, the preparation dries up quite quickly, which is a problem in
hot climatic conditions, so quick examination is essential.
§ In case of
HIV-positive patients, > 90% of cases may be positive by the India
ink/Nigrosin test, whereas in non-HIV cases, < 60 % positivity is seen.
Precautions
- The India
ink or Nigrosin should be shaken well before every wet mount preparation.
- The stain
should be regularly checked for contamination by examining just the stain
under a microscope.
- False
positive readings may occur with air bubbles or monocytes or neutrophils.
Air bubbles, under high power, will be hollow and will not show the
typical cell with characteristic nuclei. Monocytes and neutrophils have a
crenated margin (and not the entire margin seen in cryptococcal cell) and
will not show the characteristic refractive cell inclusions, and the
luminous halo around the cell is not well demarcated.
Rapid identification by
germ tube (GT) test
The germ tube test is
used for presumptive identification of Candida albicans. It is a rapid
screening test wherein the production of germ tubes within 2 hours in contact
with the serum is considered as indicative of Candida albicans. This
test must be validated with a CMA (corn meal agar) test.
Procedure
(1)
Ensure that the test starts with a fresh
growth from a pure culture.
(2)
Make a very light suspension of the test
organism in 0.5 ml of sterile serum (pooled human serum or fetal calf serum).
The optimum inoculum is 105-106 cells per ml.
(3)
Incubate at 37˚C for exactly 2 hours.
(4)
Place 1 drop from the incubated serum on
a slide with a cover slip. Observe under the microscope for production of GTs.
Observation:
Germ tubes represent initiation of hyphal growth, arising directly from the
yeast cell. They have parallel walls at their point of origin and are not
constricted. To record a positive, about 30% of the cells should show GT
production.
Quality
control: Suitable controls should be kept with each test; a
known strain of Candida albicans should be tested with each new batch of
serum. C. albicans and C. tropicalis are run with each group of
GT determinations to serve as positive and negative controls respectively.
Precautions:
(1)
The medium, inoculum size, temperature
of incubation, concentration of simple carbohydrates and microaerobic
conditions influence GT formation.
(2)
Increased concentration of inoculum
causes a significant decrease in the percentage of cells forming GTs. Maximum percentage
of GT formation occurs when 105-106 cells/ml are used as
inoculum. As the concentration of cells increases, the percentage of GT
formation decreases. A faintly turbid serum suspension is ideal for maximum GT
development.
(3)
Approximately 95% of clinical isolates
of C. albicans produce GTs when incubated in serum at 37˚C for 2-3
hours.
(4)
A neutral pH (7.4) facilitates maximum
development of germ tubes. Bacterial contamination may interfere with
production of germ tubes.
(5)
Antimicrobial substances in the
isolation medium may interfere with this test; human serum may contain
inhibitory substances (such as ferritin) that suppress GT development.