Infection and Drug Resistance 2020:13 2311–2321
Detection of OXA-48 Gene in Carbapenem-Resistant Escherichia coli and Klebsiella pneumoniae from Urine Samples
Sushma Gurung1 Sonali Kafle2 Binod Dhungel1 Nabaraj Adhikari1 Upendra Thapa Shrestha1
Bipin
Adhikari3 Megha Raj Banjara1 Komal
Raj Rijal1 Prakash Ghimire1
1Central Department
of Microbiology, Tribhuvan University, Kirtipur, Kathmandu, Nepal;
2Alka Hospital,
Lalitpur, Nepal;
3Centre for Tropical
Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, Oxford, UK
ABSTRACT
Introduction: Resistance to
carbapenem in Gram-negative bacteria is attributable to their ability to
produce carbapenemase enzymes. The main objective of this study was to detect the
presence of blaOXA-48 genes in
carbapenem-resistant uropathogenic Escherichia coli and Klebsiella
pneumoniae
isolated
from urine samples from patients attending Alka Hospital, Jawalakhel, Lalitpur,
Nepal.
Methods: A total of 1013
mid-stream urine samples were collected from patients with suspected urinary
tract infection (UTI) between April and September 2018. The identified isolates
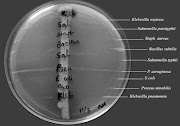
underwent antibiotic susceptibility testing using the modified Kirby–Bauer disc diffusion
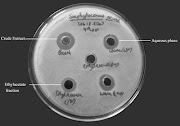
method. Phenotypic carbapenemase production was confirmed by the modified Hodge test, and
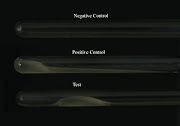
the blaOXA-48 gene was detected
using conventional polymerase chain reaction.
Results: Out of 1013 urine
samples, 15.2% (154/1013) had bacterial growth. Among the isolates, 91.5%
(141/154) were Gram-negative bacteria, and E. coli was the most common
bacterial isolate (62.9%; 97/154), followed by K. pneumoniae 15.6% (24/154).
Among 121 bacterial isolates (97 E. coli isolates and 24 K. pneumoniae isolates), 70.3%
(52/121) were multidrug-resistant E. coli and 29.7% (22/121)
were multidrug-resistant K. pneumoniae. In addition, 9.1% (11/121) were
carbapenem resistant (both imipenem and meropenem resistant). Development of
multidrug resistance and development of carbapenem resistance were significantly associated (p<0.05). Of the
11 carbapenem-resistant isolates, only seven were carbapenemase producers; of
these, 28.6% (2/7) were E. coli, 72.4% (5/7) were K. pneumoniae and 42.8% (3/7) had
the blaOXA-48 gene. Of the three
bacterial isolates with the blaOXA-48 gene, 33.3% (1/3) were E. coli and 66.7% (2/3)
were K.
pneumoniae.
Conclusion: One in ten isolates
of E.
coli and
K.
pneumoniae
were
carbapenem resistant. Among carbapenem-resistant isolates, one-third of E. coli and two-thirds of K. pneumoniae had the blaOXA-48 gene. OXA-48 serves
as a potential agent to map the distribution of resistance among clinical
isolates.
Keywords: antimicrobial
resistance, AMR, carbapenem, carbapenemase, modified Hodge test, MHT, blaOXA-48 gene
Full text article: Download