Biofilm-Producing Candida Species Causing Oropharyngeal Candidiasis in HIV
Patients Attending Sukraraj Tropical and Infectious Diseases Hospital in
Kathmandu, Nepal
Keshav Lamichhane,1,* Nabaraj Adhikari,1,* Anup Bastola,2 Lina Devkota,2 Parmananda Bhandari,2 Binod Dhungel,1 Upendra Thapa Shrestha,1 Bipin
Adhikari,3 Megha Raj Banjara,1 Komal Raj
Rijal,1 Prakash Ghimire1
1Central Department of Microbiology, Tribhuvan University,
Kathmandu, Nepal;
2Sukraraj Tropical and Infectious Disease Hospital, Teku,
Kathmandu, Nepal;
3Centre for Tropical Medicine and Global Health, Nuffield
Department of Medicine, University of Oxford, Oxford, UK
Introduction: Oropharyngeal candidiasis are the commonest fungal infections among HIV-positive patients. The main objective of this study was to explore biofilm-producing Candida species causing oropharyngeal infections among HIV patients attending Sukraraj Tropical and Infectious Diseases Hospital (STIDH) in Kathmandu, Nepal.
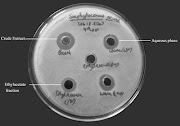
Methods: Oropharyngeal
swabs were collected from the HIV-positive patients between July and December
2019. A total of 174 oropharyngeal swabs were cultured on Sabouraud Dextrose
Agar (SDA). All samples were inoculated on SDA slants supplemented with
chloramphenicol and underwent incubation at 37°C for 24– 48 hours. Any visible
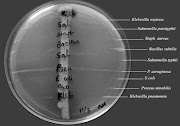
growth reported was processed for the identification of the species. Candida species were differentiated based on the growth and
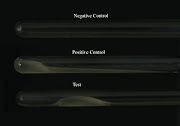
colour of the isolates on CHROM agar candida. Biofilm production in Candida species was determined by the microtiter plate method
(MPM). Antifungal susceptibility testing was performed using the disc diffusion
method.
Results: Among 174
oropharyngeal samples, 23.6% (n=41/174) of them had oropharyngeal infections
and 36.6% of the oropharyngeal infections (15/41) had CD4 T-lymphocytes count
below 200 cells/mm3 who were also active tobacco users (p< 0.05). Among
Candidial growth, 61% (25/41) were Candida albicans and 39%
(16/41) were non-albicans. Of 41 Candida spp., 65% (27/41) were biofilm producers. An equal
proportion of Candida albicans (4 isolates) and non-albicans (4 isolates) were strong
biofilm producers. C. albicans isolates were sensitive towards clotrimazole (96%;
24/25) and fluconazole (92%; 23/25), whereas sensitivity towards ketoconazole
was only 48% (12/25). Non-albicans Candida was highly sensitive to amphotericin-B (62.5%; 10/16)
followed by clotrimazole (56.2%; 9/16). The biofilm-producing Candida isolates showed the highest resistivity (51.9%; 14/27)
to ketoconazole and lowest (22.2%; 6/27) to clotrimazole.
Conclusion: Oropharyngeal candidiasis is a common opportunistic infection among HIV-infected individuals. The majority of cases of oropharyngeal candidiasis are caused by biofilm producers Candida albicans and non-albicans Candida. Biofilm producers Candida were more resistant towards commonly used antifungal drugs.
Keywords: Oral candidiasis, HIV, Candida albicans, Biofilm, Antifungal susceptibility test
HIV/AIDS - Research and Palliative Care 2020:12 211–220
For Citation and Full-Text article: Download