on
OCCURRENCE OF β-LACTAM RESISTANT BACTERIAL GENES FROM
CLINICAL, ENVIRONMENTAL AND POULTRY ISOLATES
ABSTRACT
The widespread and irrational use
of antibiotics is rampant in many parts of the world including Nepal. In
addition, the use of antibiotics in the growth of food animals in veterinary
practice and food preparation is of grave concern these days. These all factors
contribute to the emergence of drug-resistant strains of bacteria which possess
a problem in therapeutic management. Besides, the regular reporting of the
increased resistance among the strains of pathogenic microorganisms from
different clinical specimens, the higher resistance of antibiotics among the
bacterial pathogens from wastewater and poultry have been published by many
authors. However, reporting of the resistance genes from those isolates was not
documented in our contest. Hence, this study was conducted to find the
distribution pattern of resistance genes among the bacterial isolates from
different sources including clinical, animal and environmental samples. For
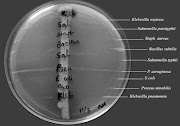
this work, bacterial pathogens such as Staphylococcus aureus, Escherichia
coli and Pseudomonas aeruginosa will be isolated separately from
clinical specimens, wastewater and poultry samples. These organisms were then subjected to
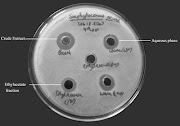
antimicrobial susceptibility testing using the modified Kirby Bauer disc diffusion
method as described in CLSI guidelines. The pathogens were further subjected to
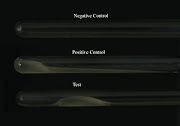
screening of resistance genes including blaTEM, mcr-1,
mecA and blaNDM-1 genes using conventional PCR. Out of
1245 clinical samples including blood, pus and wound, 80 S. aureus were
isolated and 47.5 % (38) of them were methicillin-resistant S. aureus. A
total 32 (84.2%) MRSA isolates possess mecA gene. Likewise, we observed
89 (15.3%) S. aureus from a study at different hospital among pus
specimens. Of which, 38 were MRSA and 23
of them carry mecA gene. On the other hand, the occurrence of mcr-1
gene among E. coli isolates was found to be 91.6% and 44% from clinical
and poultry origins respectively. Most of E. coli isolates from
different origins were ESBL producers carrying 41.2% of the blaTEM gene from the clinical origin and 57.5% of blaTEM gene from the water samples. The mecA gene was also
found to be higher (46.7%) among MRSA isolates from water samples. Although P.
aeruginosa isolated from the clinical specimens in our study showed
resistance to most of the antibiotics used, the occurrence of blaNDM-1
gene was lower (17.8%) as compared to other resistant genes. The resistant
genes were found to be ubiquitous among bacterial pathogens from different
sources. Moreover, the presence of those genes in transposons or plasmid DNA
indicates the potential threat of horizontal gene transfer and the emergence of
superbugs. Hence, it is an important issue to address one health concept and
alert the policymakers to formulate strict antibiotic prescription policy in the
clinical settings, prohibition of the direct disposal of hospital waste or
antimicrobial waste to the environment and strict avoidance of antibiotics uses
in animal feeds and farmings. We all should be aware that without the good
health of animals and the environment, we can't think about our good health.
Keywords: Antimicrobial resistance, MRSA, ESBL, MBL, Resistant genes (mecA, mcr-1, blaTEM, blaNDM-1)