Characteristics of Staphylococcus aureus Isolated From Clinical Specimens in a Tertiary Care Hospital, Kathmandu, Nepal
Shesh Narayan Kandel1†, Nabaraj Adhikari2†, Binod Dhungel2, Upendra Thapa Shrestha2, Khadga Bikram Angbuhang1, Gayatri Karki3, Bipin Adhikari4, Megha Raj Banjara2, Komal Raj Rijal2, Prakash Ghimire2
1Kantipur College of Medical Sciences,
Tribhuvan University, Sitapaila, Kathmandu, Nepal
2Central Department of Microbiology, Tribhuvan
University, Kirtipur, Kathmandu, Nepal
3Himal Hospital, Naxal, Kathmandu, Nepal
4Nepal Community Health and Development Centre,
Balaju, Kathmandu, Nepal
Citation: Kandel et al. Microbiology Insights, 2020, 13: 1–6. DOI: 10.1177/1178636120972695
Article first
published online: November 11, 2020; Issue published: January 1,
2020
Received: April 27, 2020; Accepted: October 16, 2020
https://creativecommons.org/licenses/by-nc/4.0/This
article is distributed under the terms of the Creative Commons
Attribution-NonCommercial 4.0 License (https://creativecommons.org/licenses/by-nc/4.0/)
which permits non-commercial use, reproduction and distribution of the work
without further permission provided the original work is attributed as
specified on the SAGE and Open Access pages (https://us.sagepub.com/en-us/nam/open-access-at-sage).
Abstract
Methicillin resistant Staphylococcus
aureus (MRSA) is a major human pathogen associated with nosocomial and
community infections. mecA gene is considered one of the important
virulence factors of S. aureus responsible for acquiring
resistance against methicillin. The main objective of this study was to explore
the prevalence, antibiotic susceptibility pattern, and mec A
gene.
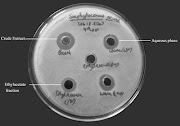
A total of 39 isolates of S.
aureus were isolated from 954 clinical specimens processed in
Microbiology laboratory of Himal Hospital, Kathmandu. Antimicrobial susceptibility
test (AST) was performed by Kirby-Bauer disc diffusion method using cefoxitin,
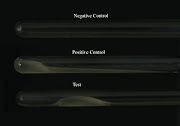
and performed Polymerase Chain Reaction (PCR) for amplification of mecA gene
in MRSA isolates.
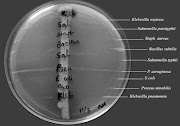
Out of 954 clinical samples, (16.2%;
153/954) samples had bacterial growth. Among 153 culture positive isolates,
25.5% (39/153) were positive for S. aureus. Among 39 S.
aureus (61.5%; 24/39) were multiple drug resistant (MDR). On AST,
amoxicillin was detected as the least effective while vancomycin was the most
effective. The prevalence of methicillin resistance was 46% (18/39) of which
72.2% (13/18) were positive for mecA gene in PCR assay.
One in 4 culture positive isolates from
the clinical specimens were S. aureus, of which almost two-thirds
were MDR. Around half of the MDR showed MRSA and significant proportion of them
were positive for mecA gene. This study concludes that
the mecA gene is solely dependent for methicillin resistance
in S. aureus but the presence of gene is not obligatory. PCR
detection of the mecA gene is reliable, valid and can be suggested
for the routine use in diagnostic laboratories.
Keywords Staphylococcus aureus, MRSA, cefoxitin, mecA gene
PUBMED: Download
SAGE HomePage: Download PDF