Factors
affecting microbial spoilage of pharmaceutical products
By
understanding the influence of environmental parameters on microorganisms, it
may be possible to manipulate formulations to create conditions which are as
unfavorable as possible for growth and spoilage, within the limitations of
patient acceptability and therapeutic efficacy.
Types
and size of contaminant inoculum
When
failures inevitably occur from time to time, knowledge of the microbial ecology
and careful identification of contaminants can be most useful in tracking down
the defective steps in the design or production process. Low levels of
contaminants may not cause appreciable spoilage, if unable to replicate in a
product; however, an unexpected surge in the contaminant bioburden may present
an unacceptable challenge to the designed formulation. This could arise as if
there was a lapse in the plant-cleaning protocol; a biofilm detached itself
from within supplying pipework; or the product had been grossly misused during
administration. Inoculum size alone is not always a reliable indicator of
likely spoilage potential. Low levels of aggressive pseudomonads in a weakly
preserved solution may suggest a greater risk than tablets containing fairly
high numbers of
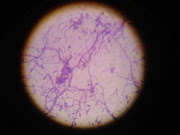
fungal
and bacterial spores.
When
an aggressive microorganism contaminates a medicine, there may be an
appreciable lag period before significant spoilage begins, the duration of
which decreases disproportionately with increasing contaminant loading. As
there is usually a considerable delay between manufacture and administration of
factory-made medicines, growth and attack could ensue during this period unless
additional steps were taken to prevent it.
The
isolation of a particular microorganism from a markedly spoiled product does
not necessarily
mean
that it was the initiator of the attack. It could be a secondary opportunist
contaminant which had overgrown the primary spoilage organism once the physicochemical
properties had been favourably modified by the primary spoiler.
Nutritional
factors
Microorganisms
enable them to utilize many formulation components as substrates for
biosynthesis and growth. The use of crude vegetable or animal products in a
formulation provides an additionally nutritious environment. Even demineralized
water prepared by good ion-exchange methods will normally contain sufficient
nutrients to allow significant growth of many waterborne Gram-negative bacteria
such as Pseudomonas spp. When such contaminants fail to survive, it is
unlikely to be the result of nutrient limitation in the product but due to other,
non-supportive, physicochemical or toxic properties.
Acute
pathogens require specific growth factors normally associated with the tissues
they infect but which are often absent in pharmaceutical formulations. They are
thus unlikely to multiply in them, although they may remain viable and
infective for an appreciable time in some dry products where the conditions are
suitably protective.
Moisture
content: water activity (Aw)
Microorganisms
require readily accessible water in appreciable quantities for growth to occur.
By measuring a product’s water activity (Aw), it is possible to
obtain an estimate of the proportion of uncomplexed water that is available in
the formulation to support microbial growth, using the formula: Aw
= vapour pressure of formulation/vapour pressure of water under similar
conditions.
The
greater the solute concentration, the lower is the water activity. With the
exception of halophilic bacteria, most microorganisms grow best in dilute solutions
(high Aw) and, as solute concentration rises (lowering Aw),
growth rates decline until a minimal growth-inhibitory Aw, is reached.
The
Aw of aqueous formulations can be lowered to increase resistance to
microbial attack by the addition of high concentrations of sugars or polyethylene
glycols. Aw can also be reduced by drying, although the dry, often
hygroscopic medicines (tablets, capsules, powders) will require suitable
packaging to prevent resorption of water and consequent microbial growth.
Condensation
similarly formed on the surface of viscous products such as syrups and creams,
or exuded by syneresis from hydrogels, may well permit surface yeast and fungal
spoilage.
Redox
potential
The
ability of microbes to grow in an environment is influenced by its
oxidation-reduction balance (redox potential), as they will require compatible terminal
electron acceptors to permit their respiratory pathways to function. The redox
potential even in fairly viscous emulsions may be quite high due to the
appreciable solubility of oxygen in most fats and oils.
Storage
temperature
Spoilage
of pharmaceuticals could occur potentially over the range of about -20°C to
60°C, although it is much less likely at the extremes. The particular storage
temperature may selectively determine the types of microorganisms involved in
spoilage. A deep freeze at -20°C or lower is used for long-term storage of some
pharmaceutical raw materials and short-term storage of dispensed total
parenteral nutrition (TPN) feeds prepared in hospitals. Reconstituted syrups
and multi-dose eye-drop packs are sometimes dispensed with the instruction to
‘store in a cool place’ such as a domestic fridge (8°–12°C), partly to reduce
the risk of growth of contaminants inadvertently introduced during use.
Conversely, Water for Injections (EP) should be held at 80°C
or
above after distillation and before packing and sterilization to prevent
possible regrowth of Gram negative bacteria and the release of endotoxins.
pH
Extremes
of pH prevent microbial attack. Around neutrality,
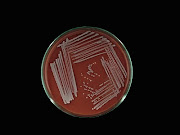
bacterial spoilage is more likely, with reports of pseudomonads and related Gram-negative
bacteria growing in antacid mixtures, flavoured mouthwashes and in distilled or
demineralized water. Above pH 8 (e.g. with soap-based emulsions) spoilage is
rare. In products with low pH levels (e.g. fruit juice-flavoured syrups with a
pH 3–4), mould or yeast attack is more likely. Yeasts can metabolize organic
acids and raise the pH to levels where secondary bacterial growth can occur.
Although the use of low pH adjustment to preserve foodstuffs is well
established (e.g. pickling, coleslaw, yoghurt), it is not practicable to make
deliberate use of this for medicines.
Packaging
design
Packaging
can have a major influence on microbial stability of some formulations in
controlling the entry of contaminants during both storage and use. Considerable
thought has gone into the design of containers to prevent the ingress of
contaminants into medicines for parenteral administration, owing to the high
risks of infection by this route. Self-sealing rubber wads must be used to
prevent microbial entry into multi-dose injection containers following
withdrawals with a hypodermic needle.
Where
medicines rely on their low Aw to prevent spoilage, packaging
such as strip foils must be of water vapour-proof materials with fully efficient
seals. Cardboard outer packaging and labels themselves can become substrates
for microbial attack under humid conditions, and preservatives are often
included to reduce the risk of damage.
Protection
of microorganisms within pharmaceutical products
The
survival of microorganisms in particular environments is sometimes influenced
by the presence of relatively inert materials. Thus, microbes can be more
resistant to heat or desiccation in the presence of polymers such as starch,
acacia or gelatin. Adsorption onto naturally occurring particulate material may
aid establishment and survival in some environments. There is a belief, but
limited hard evidence, that the presence of suspended particles such as kaolin,
magnesium trisilicate or aluminium hydroxide gel may influence contaminant
longevity in those products containing them, and that the presence of some
surfactants, suspending agents and proteins can increase the resistance of
microorganisms to preservatives, over and above their direct inactivating effect
on the preservative itself.