Friday, July 30, 2021
1. Different vaccines for Dengue and their efficacy
Around 390 million Dengue viral infections occur annually and out of which 96 million people are clinically ill with sign and symptoms caused by four different serotypes of dengue viruses (Dengue virus serotype 1, DENV1, DENV2, DENV3 and DENV4). However, there is no any specific medicine for treatment till date. The only mean of control for dengue virus infection is control of vector. Vaccines in the other way have been developed for the prevention of dengue infections. Many of vaccines are under the clinical trials while one of them has already been licensed in Asia and Latin America instead of few minor drawbacks (da Silveira et al., 2019; Deng et al., 2020).
An ideal dengue vaccine candidate should have at least target
to all four serotypes of dengue viruses; DENV1 to DENV4 (tetravalent). The
candidate vaccine should be low reactogenic, highly immunogenic providing
lifelong immunogenicity, effective with minimal or no repeat immunizations,
minimize the cost of production and finally should have high efficacy. Except
few vaccines, most of the vaccines couldn’t meet these requirements because of
which only a few vaccines are under the progress.
Till now, five different types of vaccines have been
developed. These are live attenuated vaccines, inactivated vaccines,
recombinant subunit vaccines, viral vectored vaccines and DNA vaccines. All of
the vaccines act primarily by increasing immune responses against dengue virus
envelope (E) protein and non-structural protein (NS-1). Two major challenges have been faced in the
course of ideal vaccine development. The first one is the antibody dependent
enhancement (ADE-related complications) related complications which may lead to
dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS) among the
seronegative children of less than 9 years. This effect is seen resulting from
a second heterotypic infection (infection from different serotype) in which the
preformed neutralizing antibodies against cross reactive serotype are not
sufficient to neutralize the new serotype. Secondly, there is lack of
conveniently accessible cheap and sensitive animal models capable of
stimulating the immune response in human after infections by vaccines. Since
mice are naturally resistant to DENV infections and non-human primates are good
animal model but very expensive to use in the experiment. Because of which
vaccines have to be tested on human cell chimeric mice and immunodeficient mice
that are comparatively less convenient for vaccines evaluation (da Silveira
et al., 2019; Deng et
al., 2020).
The live attenuated vaccines contain antigenic substances
composed of living viruses making them weak or avirulent. They will deliver a
set of protective antigens. The immune responses against those antigens provide
long term immune protectivity to host. Chimeric yellow fever 17D
virus-tetravalent dengue vaccine (CYD-TDV) commercially known as Dengvaxia,
recombinant DENV4 mutant bearing a 30-nucleotide deletion vaccine (rDEN4D30) and tetra-live attenuated virus
dengue vaccine (DENVax) are examples of live attenuated vaccines. The
only licensed dengue vaccine is Sanofi Pasteur’s Dengvaxia®(CYD-TDV)
which is constructed by replacing prM/E RNAs of Yellow fever virus vaccine
strain (YE 17D) with the structural pre-membrane (prM) and envelop (E) genes
from all four serotypes of dengue virus. Recently, the vaccine has been registered
in 20 dengue endemic countries, however, immunization was implemented in only
two countries, Brazil and the Philippines. The vaccines are highly effective
among the children older than 9 years and the immunity lasts for 4 years. The
efficacy of the vaccine is however influenced by the age, virus serotypes and
immune status of children (seropositive or seronegative) at the time of
immunization. Due to higher risk of ADE related complication and increased
hospitalization among the seronegative cases, WHO Strategic Advisory Panel-2018
updated the need of priority screening of DENV serostatus before vaccination.
The problem is still unsolved because of sensitivity and specificity of rapid
diagnostic kits used for prior screening of dengue infections (Deng et al.,
2020; Thomas and Yoon, 2019)
Although only CYD-TDV vaccine has been licensed till date,
many more vaccines are on the way of progressing at different phases in
clinical trials. Inactivated virus
vaccines are safer to use but less immunogenic. They are prepared from
inactivated materials; capsid (C), membrane (M), envelop (E) and NS1 proteins
from the viruses which can stimulate the immune response. The protectivity of
such vaccines are poor. DEN2 inactivated vaccines S16803 prepared from formalin
inactivation fails to arise stable antibody titers in rhesus monkey. The other
inactivated vaccines; tetravalent purified formalin inactivated virus vaccine
(TPIV) containing inactivated dengue serotypes or tetravalent DNA vaccine
enhance the humoral immunity when given with live attenuated vaccines. Likewise,
recombinant subunit vaccines are composed of antigenic proteins which are
expressed by prokaryotic and eukaryotic cells. The expression of antigens in E.
coli is easy but there is a problem of endotoxin contamination or
misfolding of proteins in different organisms. These proteins are quite
protective in mice. Tetravalent recombinant subunit vaccines when given with
alum adjuvant elicit DENV2 antibodies in macaques. EDIII-P64K contains P64K
antigens expressed in Neisseria meningitidis and EDIII of different dengue
serotypes. The vaccines induce high tires of DENV1-DENV3 antibodies but low
titre of DENV4 antibodies. The viral vectored vaccines use Vaccinia, Adeno and
Alphavirus as vectors to express DENV antigens prM, E, NS1 and NS2A proteins.
The non-attenuated (WR) cidofobir resistant vaccinia strain is used as safe vector
but induce low level of specific antibodies against the E protein in mice. Among
the virus vectors, Adeno virus is easier in gene manipulation and high level of
protein expression while Alphavirus has high potential and high level of
antigen expression in a single round of vaccination. The last one is DNA vaccine
which is composed of a plasmid containing one or more genes encoding specific
antigens of viruses. The plasmid is used to expressed prM and E proteins of
virus. E80 vaccine expressing 80% E protein shows less immunogenic than EM100
which expresses prM protein and 100% E protein. In human test, D1ME100 showed
safe and well tolerated. DNA vaccine alone induced a moderate level of neutralizing
antibodies while it combined with recombinant proteins induced higher titers of
antibodies. Despite of its stability, easy in preparation and low cost, DNA
vaccines lack high immunogenicity (Deng et al., 2020; Thomas
and Yoon, 2019).
As
described above, there are five types of vaccines against DENV each type has
its own pros and cons. Among the dengue vaccine candidates, live attenuated
tetravalent dengue vaccine (CYD-TDV) can stimulate neutralizing antibodies in
humans, but response to DENV2 virus is low. Many studies also reported ADE
related hospitalization among immunized children. The other live attenuated
vaccine, DENV monovalent vaccines with
live attenuated tetravalent vaccines (LATV); rDEN4D30 and Live attenuated chimeric tetra Dengue vaccines;
DENV2 PDK-53 (DENVax) have attempted to overcome the problem of adverse effects
and high level of induced immune balance. They are somehow succeeded as well
but they need to be evaluated more. These vaccines are under phase III clinical
trials and not on the way of pilot survey. Despite of few drawbacks of
Dengvaxia vaccine, it is succeeded to reduce mortality and morbidity by dengue
infection in endemic regions. Hence, WHO also approved this vaccine but with updated
strategic plan for screening of serostatus of vaccinees. On the basis of the
results from clinical trials, the vaccine is no doubt in superiority with other
vaccines. Regarding the safety and immunogenicity studies, Dengvaxia’s® acute safety
profile was found to be similar to licensed Yellow fever vaccine and not
affected by pre-existing Yellow fever immunity. In three clinical endpoint
studies, Dengvaxia® maintained the positive acute safety and reactogenicity
profile established in early clinical studies. In conclusion, the vaccine is safe, highly immunogenic and low
reactogenic with satisfactory efficacy. The vaccine contains no
adjuvant or preservatives or material of porcin origin, highly stable and
available in powder form with separate solvent (Rosa et al., 2019; Thomas and
Yoon, 2019). Till now there is no any other vaccines which can meet such
criteria to be an ideal vaccine, therefore in current scenario, CYD-TDV
(Dengvaxia) is the best vaccines for control of dengue infections.
References:
1.
da Silveira LTC, Tura B, and Santos M. Systematic review of dengue vaccine
efficacy. BMC
Infectious Diseases. 2019; 19: 750.
2.
Deng S, Yang X, Wei Y, Chen J, Wang X, and Peng H. A Review
on Dengue Vaccine Development. Vaccines. 2020; 8: 63. doi:10.3390/vaccines8010063.
3.
Rosa BR, Cunha AJLA, and Medronho RA. Efficacy,
immunogenicity and safety of a recombinant tetravalent dengue vaccine (CYD-TDV)
in children aged 2–17 years: systematic review and meta-analysis. BMJ Open. 2019; 9: e019368.
doi:10.1136/bmjopen-2017-019368.
Biofilm Formation and Phenotypic Detection of ESBL, MBL, KPC and AmpC Enzymes and Their Coexistence in Klebsiella spp. Isolated at the National Reference Laboratory, Kathmandu, Nepal
Biofilm Formation and Phenotypic Detection of ESBL, MBL, KPC and AmpC Enzymes and Their Coexistence in Klebsiella spp. Isolated at the National Reference Laboratory, Kathmandu, Nepal
Susmita Kuinkel1, Jyoti Acharya2, Binod
Dhungel1, Sanjib Adhikari1, Nabaraj Adhikari1,
Upendra Thapa Shrestha1, Megha Raj Banjara1, Komal
Raj Rijal1, * and Prakash Ghimire1
1Central
Department of Microbiology, Tribhuvan University, Kirtipur, Kathmandu, Nepal
2National
Public Health Laboratory, Teku, Kathmandu, Nepal
* Correspondence: rijalkomal@gmail.com or
komal.rijal@cdmi.tu.edu.np
ABSTRACT
Klebsiella spp. are associated with several nosocomial and
opportunistic infections. Increasing antimicrobial resistance of Klebsiella
species is aggravated by a number of intrinsic and extrinsic factors. The main
aim of this study is to determine antimicrobial resistance due to production of
β-lactamase enzymes, extended spectrum beta-lactamase (ESBL),
metallo-beta-lactamase (MBL) and AmpC and Klebsiella pneumoniae carbapenemase
(KPC) and biofilm formation in Klebsiella isolates. A total of 2197
non-duplicate specimens of urine, sputum and pus were obtained from the
National Public Health Laboratory (NPHL), Kathmandu, Nepal, between February
and August 2019. Klebsiella species were isolated, identified and
screened for antimicrobial susceptibility testing with the disk diffusion
method. Phenotypic detection of ESBL, MBL, KPC and AmpC production was observed
and biofilm production was detected by the microtiter plate method. Out of a
total of 2197 clinical specimens, bacterial growth was detected in 8%
(175/2197) of the specimens. Of the total isolates, 86.3% (151/175) were
Gram-negative bacteria and 37.7% (57/151) were Klebsiella spp. Of the
total Klebsiella spp., 56% (32/57) were multi drug resistant (MDR), 16%
(9/57) were ESBL, 26% (15/57) were MBL, 4% (2/57) were KPC (class A
carbapenemase), 16% (9/57) were AmpC producers and 95% (54/57) were biofilm
producers. Gentamicin was the most effective antibiotic, followed by
cotrimoxazole, as 68% (39/57) and 47% (27/57) of the Klebsiella isolates
were susceptible towards these drugs, respectively. The study results show
evidence of β-lactamase production, high prevalence of MDR and biofilm
producing Klebsiella species. Integrating the test parameters for
phenotypic confirmation of ESBL, MBL, AmpC β lactamase and KPC in routine
diagnostic procedures can help in the early detection and management of these
resistant strains.
Keywords: Antimicrobial resistance; Multi drug resistant (MDR); Extended-spectrum
β-lactamase (ESBL); AmpC β-lactamase (ABL); Carbapenemase; Biofilm
Citation: Kuinkel, S.; Acharya, J.; Dhungel, B.; Adhikari, S.; Adhikari, N.; Shrestha, U.T.; Banjara, M.R.; Rijal, K.R.; Ghimire, P. Biofilm Formation and Phenotypic Detection of ESBL, MBL, KPC and AmpC Enzymes and Their Coexistence in Klebsiella spp. Isolated at the National Reference Laboratory, Kathmandu, Nepal. Microbiol. Res. 2021, 12, 683–697. https://doi.org/10.3390/microbiolres12030049, www.mdpi.com/journal/microbiolres
For Full text: Download
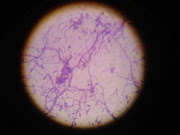
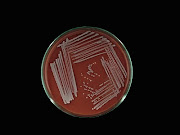
Bacteria in Photos